General Principles:
1. Patient History: Obtain a detailed history, including mechanism of injury, energy level, and patient-specific factors (e.g., age, bone quality).
2. Comprehensive Examination:
Conduct a thorough clinical exam, assessing neurovascular status, range of motion, ligamentous stability, and soft tissue integrity.
3. Advanced Imaging: Utilize X-rays, CT scans, and potentially MRI to fully characterize the fracture pattern, displacement, articular involvement, and associated soft tissue injuries.
4. Timing of Surgery: Consider soft tissue status, swelling, and patient factors when deciding on immediate vs. staged surgery. Urgent intervention may be needed for open fractures, compartment syndrome, or vascular compromise.
5. Goals of Surgery: Aim to restore articular congruency, joint stability, axial alignment, and limb length for optimal long-term function and minimize the risk of post-traumatic arthritis.
6. AO Principles: Adhere to fundamental principles of anatomical reduction, stable internal fixation, atraumatic surgical technique, and early mobilization whenever possible.
Understanding Fracture Patterns:
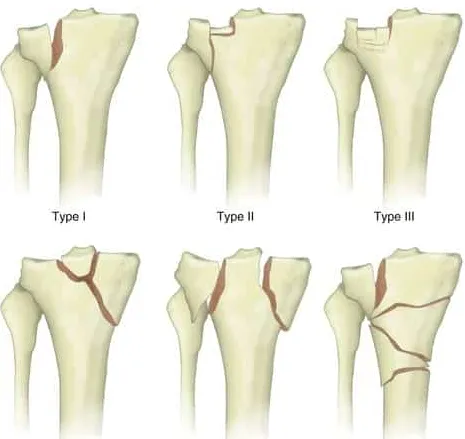
1. Schatzker Classification:
Schatzker Familiarize yourself with the Schatzker classification system to categorize tibial plateau fractures based on their complexity and morphology.
2. Mechanism of Injury: Understanding the direction and magnitude of forces involved helps predict common fracture patterns and potential soft tissue injuries.
3. Split Wedge Concept: Recognize that the split wedge fragment, defined by its three-dimensional characteristics, is often the primary determinant of joint stability and dictates the surgical approach.
4. Tibial Rim Continuity: Restoring anatomical alignment and fixation of the split wedge fragment is crucial for re-establishing tibial rim continuity and overall joint stability.
5. Three-Dimensional Understanding:
Utilize CT scans to accurately visualize fracture lines in all three planes (axial, coronal, and sagittal) for comprehensive preoperative planning.
6. Cartilage vs. Non-Cartilaginous Areas:
Prioritize anatomical reduction for cartilage-covered articular surfaces involved in weight-bearing and joint congruity. Minor displacement in non-articular areas may be acceptable.
Surgical Approach Selection:
1. Approach Based on Fracture:
Tailor the surgical approach based on the specific fracture pattern, location of the split wedge, and necessary fixation points, ensuring adequate visualization and access.
2. Minimally Invasive Options:
Consider percutaneous or minimally invasive plate osteosynthesis (MIPO) techniques for select fracture patterns to minimize soft tissue disruption, reduce postoperative pain, and potentially facilitate faster recovery.
3. Dual Approaches: Combined approaches (e.g., anterolateral and posteromedial) may be required for complex bicondylar fractures to achieve optimal visualization, reduction, and fixation of both plateaus.
Specific Approaches:
1. Anterolateral Approach: Most commonly used approach, suitable for lateral plateau fractures, allowing access to the lateral meniscus and joint line. Limited for addressing posterolateral fragments.
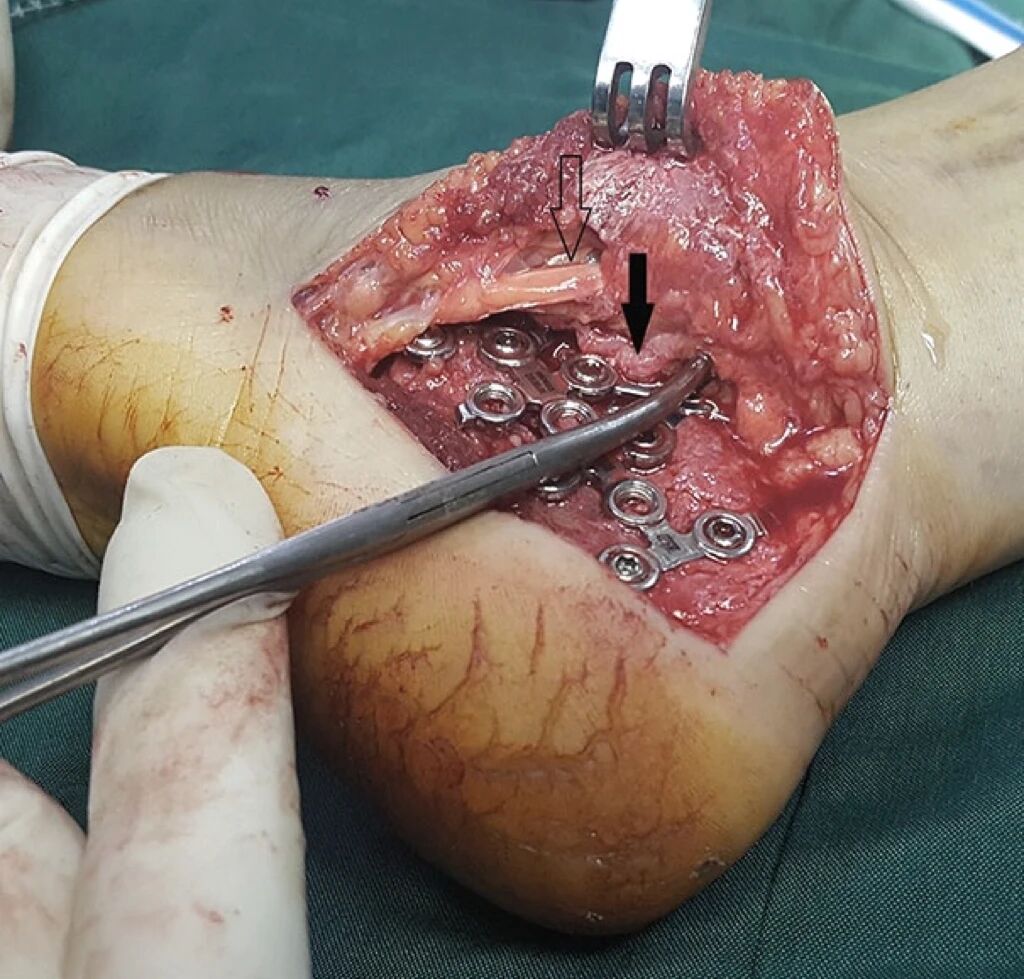
2. Posterolateral Approach: Technically more demanding approach ideal for addressing posterior displacement and posterolateral fragments. Carries higher risks of neurovascular injury (common peroneal nerve).
3. Medial Approach: Utilized for anteromedial fractures, providing access to the medial meniscus and joint line. Direct articular visualization can be limited without detaching the medial collateral ligament (MCL).
4. Posteromedial Approach: Valuable for managing shear or coronal fractures of the medial plateau. Allows for placement of antiglide plates to counteract medial displacement forces. Can be performed in supine or prone positions.
5. Direct Posterior Approach:
Rarely used, typically reserved for specific posterior bicondylar patterns or cases requiring extensive posterior exposure. Carries the highest risk of neurovascular injury (popliteal artery and tibial nerve).
Fracture Reduction and Fixation:
1. Restore Stability First: Prioritize anatomical reduction and stabilization of the split wedge fragment to re-establish joint stability before addressing other fracture components.
2. Address Articular Depression:
Elevate depressed articular fragments using minimally invasive techniques (e.g., bone tamp, minimally invasive distractors) and support them with structural bone grafting, bone substitutes, or a combination of both.
3. Buttress Plating: Utilize plates to buttress and contain elevated articular fragments, preventing collapse and maintaining reduction. Choose the plate type (e.g., locking, non-locking, pre-contoured) based on fracture characteristics.
4. Plate Positioning: Position plates strategically based on the fracture pattern and desired buttressing effect. Avoid placing plates directly beneath articular surfaces to prevent implant prominence and optimize soft tissue healing.
5. Screw Selection: Utilize appropriate screw types (e.g., locking screws for osteoporotic bone, non-locking screws for improved compression) and sizes for optimal fixation while respecting surrounding anatomical structures.
Special Considerations:
1. Posteromedial Fractures: Often technically challenging due to their inherent instability and proximity to critical neurovascular structures. Meticulous reduction and stable fixation are crucial to counteract deforming forces.
2. Posterolateral Controversy:
The significance of posterolateral fragments remains a topic of debate. Carefully consider the degree of displacement, articular involvement, and impact on overall stability before pursuing aggressive fixation.
3. Pure Depression Fractures:
For pure depression fractures without a distinct split wedge, focus on restoring articular congruity while preserving subchondral bone viability to promote optimal healing and cartilage health.
4. Osteoporotic Bone: Fractures in osteoporotic bone require careful handling to avoid iatrogenic fracture extension. Consider augmented fixation techniques (e.g., locking plates, cement augmentation) to achieve adequate implant purchase and prevent cutout.
5. Soft Tissue Management: Minimize further soft tissue damage with atraumatic surgical technique, careful handling of tissues, and respect for surrounding neurovascular structures. Consider staged procedures if significant swelling or soft tissue compromise exists.
Postoperative Care:
1. Pain Management: Implement multimodal pain management strategies to optimize patient comfort and early mobilization.
2. Early Motion: Encourage early, protected range of motion exercises as tolerated to prevent joint stiffness, promote soft tissue healing, and restore knee function.
3. Weight-Bearing Progression:
Advance weight-bearing gradually based on fracture stability, fixation strength, patient factors, and clinical progress. Early weight-bearing may not be appropriate for all fracture types.
4. Rehabilitation Protocol: Implement a structured rehabilitation program tailored to the individual patient and fracture characteristics to restore strength, range of motion, proprioception, and functional independence.
5. Long-Term Follow-Up: Monitor patients long-term for potential complications, such as post-traumatic arthritis, implant failure, or loss of reduction. Provide appropriate interventions as needed, including revision surgery or joint replacement.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!