Orthopedic surgery, though transformative for patients suffering from musculoskeletal disorders, carries an inherent risk of vascular injury. While relatively uncommon, these complications can have devastating consequences, including limb loss and even death. This article provides a detailed review of the types of orthopedic surgeries most susceptible to vascular injury, the mechanisms underlying these injuries, and the crucial preventive measures that can be employed to mitigate this risk.
Orthopedic Procedures Prone to Vascular Injury:
While any orthopedic surgery involving manipulation near major blood vessels carries some risk, certain procedures stand out as being particularly prone to vascular complications:
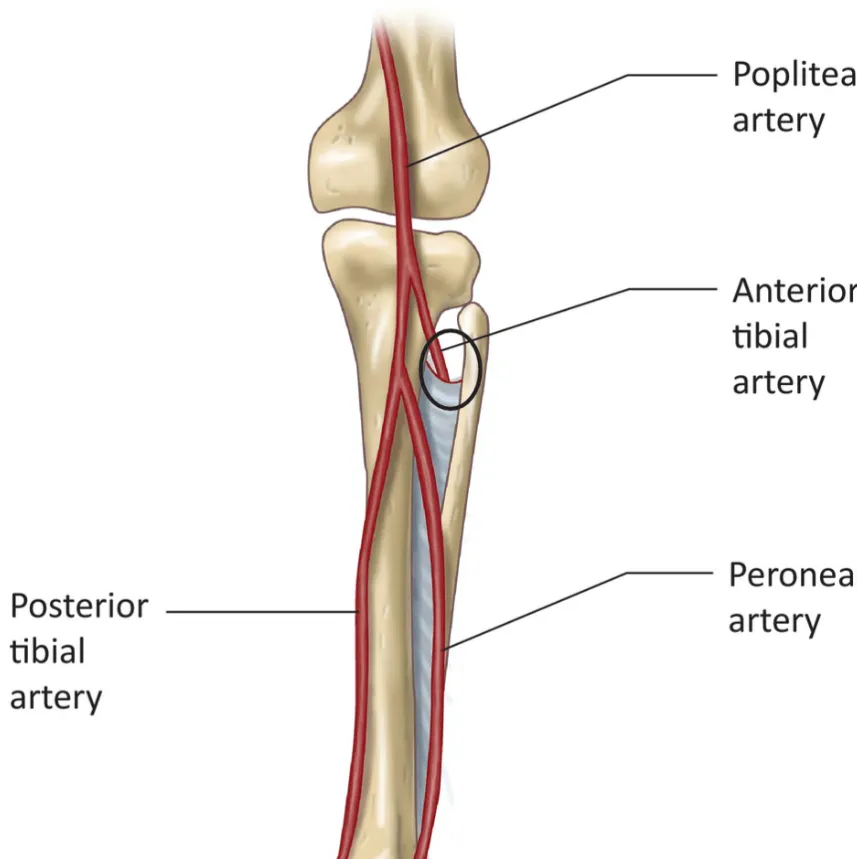
Knee Arthroplasty: This procedure has consistently been identified as the most common culprit, with reported incidence rates ranging from 0.03% to 0.17%. Revision knee arthroplasty poses an even greater risk, reaching up to 0.34%, due to the presence of dense scar tissue surrounding the popliteal vessels.
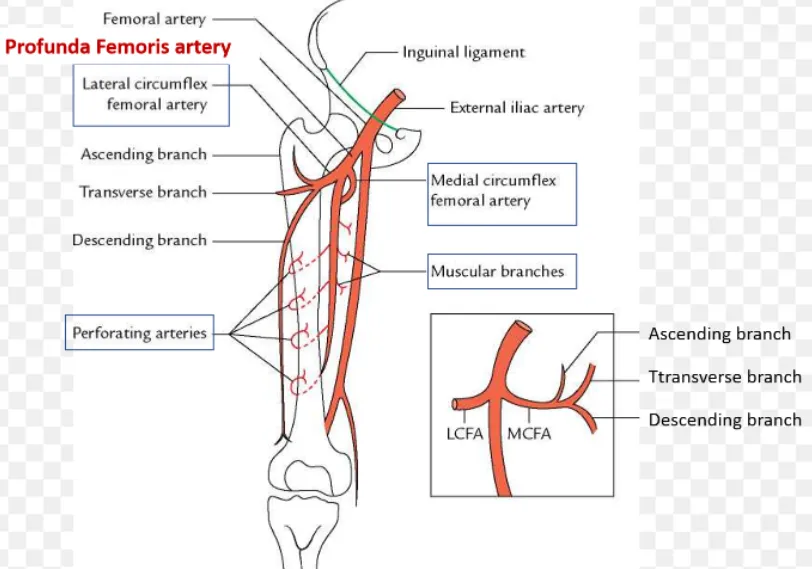
Hip Arthroplasty: Although less frequent than in knee arthroplasty, vascular injury can occur during hip procedures, with reported incidence rates ranging from 0.08% to 0.15%. The forceful impaction of the prosthesis, reaming of the femoral canal, and manipulation of the hip joint can all contribute to injury of the femoral artery, profundal femoris artery, or external iliac artery.
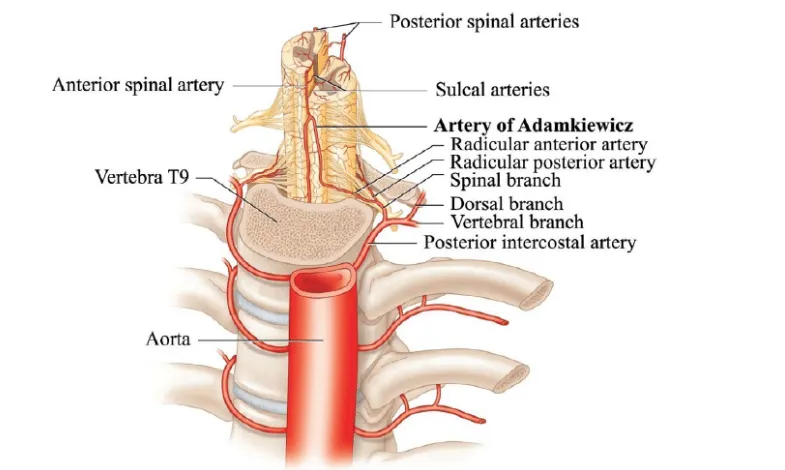
Spinal Surgery: Vascular injury during spine surgery is relatively rare, with an incidence of less than 0.05%. Anterior lumbar spinal fusion, in particular, has been associated with iliac artery thrombosis due to retraction of the vessels during exposure. Pedicle screw placement in thoracic and thoracolumbar spine surgeries carries a risk of direct injury to the aorta, though this is exceptionally rare.
Knee Arthroscopy: While the incidence is lower than in arthroplasty, vascular injury can occur during knee arthroscopy, with the popliteal artery being the most vulnerable due to its close proximity to the posterior capsule. The reported incidence is less than 1%, with most injuries occurring during meniscectomy or ligament reconstruction procedures.
Other Procedures: Other orthopedic procedures associated with vascular injury include:
Iliac Bone Graft Harvest: Injury to the superior gluteal artery or branches of the iliac artery can occur during both anterior and posterior approaches.
Shoulder Arthroplasty: Axillary artery injury can occur, particularly during revision procedures.
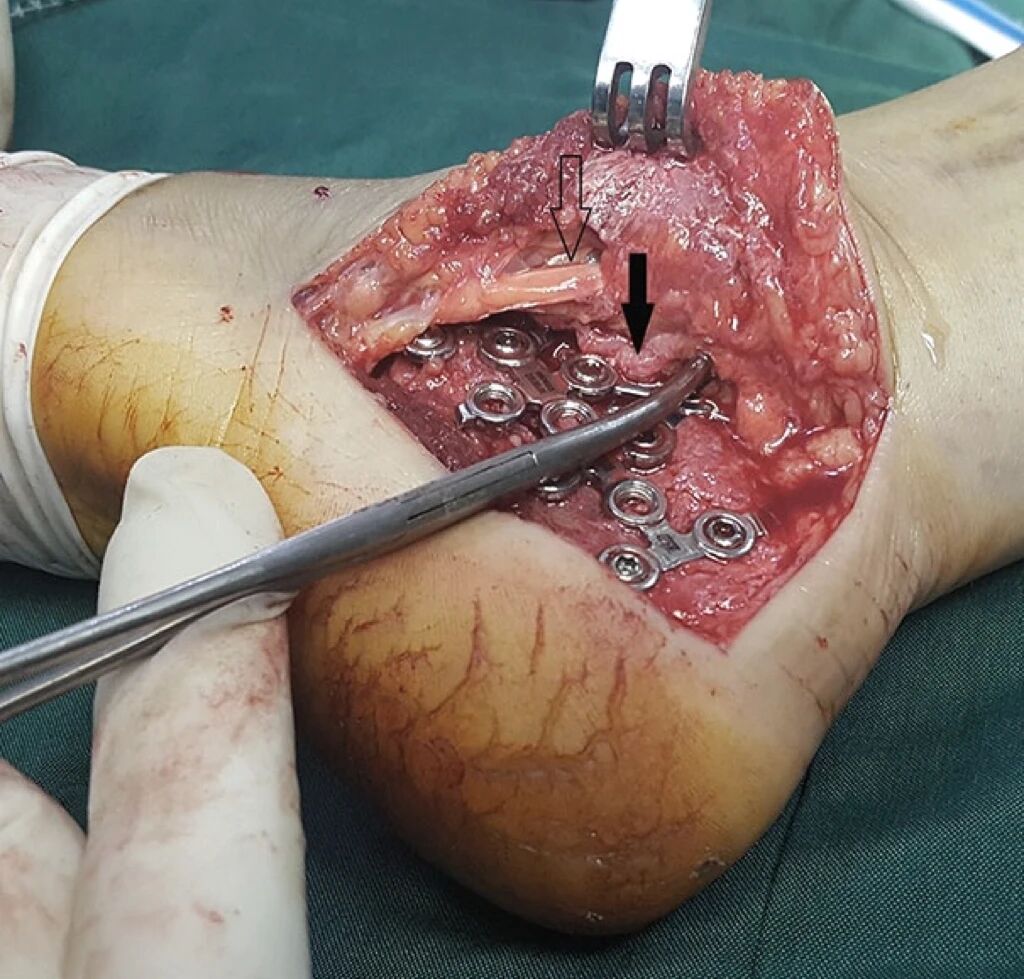
Long Bone Fracture Fixation: Although rare, injury to adjacent arteries can occur during fracture fixation, particularly in the setting of open fractures or complex fracture patterns.
Understanding the Mechanisms of Injury:
Vascular injuries during orthopedic surgery can be broadly categorized into two mechanisms:
- Direct Injury: This involves direct contact between a surgical instrument or implant and the vessel wall, leading to:
- Laceration: A full-thickness tear in the vessel wall, resulting in immediate bleeding.
- Puncture: A small hole in the vessel wall, which may initially be asymptomatic but can later develop into a pseudoaneurysm or arteriovenous fistula.
- Transaction: A complete severing of the vessel, leading to significant hemorrhage.
- Compression: Prolonged compression of a vessel, for example, by a retractor or misplaced implant, can lead to thrombosis or intimal injury.
- Indirect Injury: This encompasses damage caused by stretching, twisting, or kinking of the vessel, often due to:
- Extreme Joint Positioning: For example, forced hyperextension of the knee during knee arthroplasty can stretch and injure the popliteal artery.
- Excessive Retraction: Aggressive retraction on major vessels during surgical exposure can cause intimal tears, dissections, or thrombosis.
- Joint Manipulation: forceful manipulation of a joint, particularly during the reduction of a fracture or dislocation, can injure adjacent vessels.
Minimizing the Risk: Preventive Strategies:
Preventing vascular injury during orthopedic surgery requires a multifaceted approach that emphasizes meticulous planning, careful surgical technique, and diligent monitoring:
Preoperative Evaluation and Planning:
- Thorough Vascular Assessment: A detailed history and physical examination, focusing on vascular risk factors such as peripheral arterial disease, diabetes, smoking, and previous vascular surgery, is essential.
- Preoperative Imaging: Appropriate imaging studies, such as duplex ultrasound or CT angiography, should be obtained to assess the anatomy and health of the vessels in the operative field, particularly in patients with known vascular disease or undergoing revision surgeries.
- Multidisciplinary Consultation: When necessary, consultation with a vascular surgeon should be obtained to discuss the risks and benefits of the planned procedure and to develop a contingency plan in case of vascular injury.
Intraoperative Measures:
- Gentle Tissue Handling: Careful and atraumatic dissection techniques, minimizing the use of electrocautery near major vessels, are crucial.
- Judicious Retraction: Retractors should be placed with meticulous care, avoiding excessive pressure on major vessels. Frequent repositioning of retractors can help prevent prolonged compression.
- Optimal Joint Positioning: Extreme joint positions should be avoided whenever possible. When necessary, joint manipulation should be performed slowly and gently.
- Intraoperative Neuromonitoring: Somatosensory evoked potentials (SSEPs) monitoring can be valuable during spine surgery to detect potential compression or ischemic injury to the spinal cord and nerve roots. Sudden changes in SSEP signals may also indicate compromise of nearby arteries.
- Cementing Technique: During procedures involving bone cement, careful cementing technique is essential to prevent extravasation of cement into the surrounding tissues, which can cause vascular injury or embolization.
Postoperative Management:
- Vascular Monitoring: Diligent postoperative monitoring for signs of vascular compromise, including pain, pallor, paresthesia, diminished pulses, and cool extremities, is crucial.
- Prompt Intervention: If vascular injury is suspected, prompt evaluation by a vascular surgeon is mandatory. Diagnostic imaging, such as duplex ultrasound or angiography, should be performed to confirm the diagnosis and guide treatment.
- Treatment Options: Treatment options for vascular injuries range from observation for minor injuries to surgical repair or endovascular intervention for more significant injuries.
Conclusion:
Vascular injury in orthopedic surgery, though uncommon, represents a serious complication with potentially devastating consequences. A proactive and comprehensive approach, encompassing thorough preoperative assessment, meticulous surgical technique, and vigilant postoperative monitoring, is essential to minimize this risk. Collaboration between orthopedic surgeons, vascular surgeons, and interventional radiologists is often key to achieving optimal outcomes and ensuring patient safety.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!