Meta Description (155 chars): Clear, evidence-based guide to tibial plateau fracture weight-bearing timing—conservative vs ORIF, criteria, risks, and staged rehab that actually works.
Tibial Plateau Fracture Weight-Bearing Timing: The Evidence You Can Use Tomorrow
When it comes to tibial plateau fracture weight-bearing timing, guesswork is costly. Too early and you risk collapse; too late and you hard-wire stiffness and sarcopenia. This guide distills high-signal data into a practical, staged approach—conservative vs ORIF, imaging thresholds, and who truly qualifies for early loading. We cut through dogma and show how modern fixation and better biology are changing the rules.
Key term focus: tibial plateau fracture weight-bearing timing (used throughout to match search intent).
Understanding the Injury: Why Timing Isn’t One-Size-Fits-All
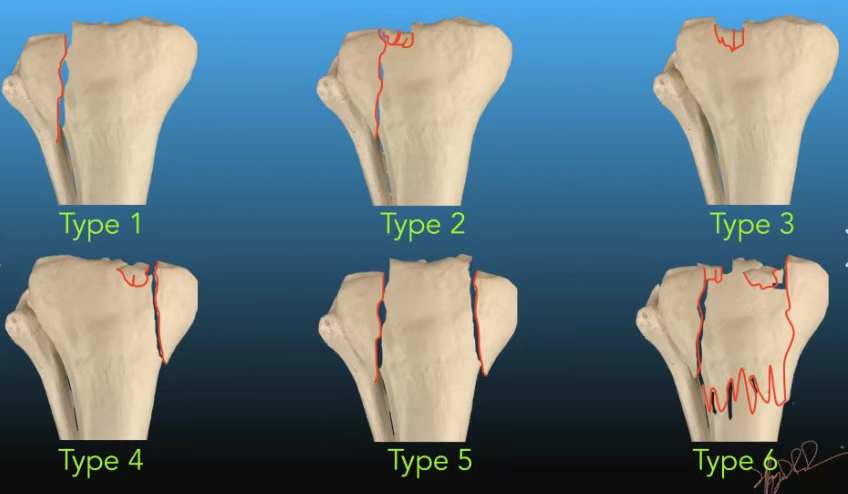
The tibial plateau is a primary load-bearing surface with dual demands—smooth articular congruity and ligamentous stability. External varus/valgus plus axial load generates classic Schatzker patterns. That’s why tibial plateau fracture weight-bearing timing must reflect:
- Pattern severity (I–VI),
- Articular step-off/condylar widening, and
- Soft-tissue status (swelling, blisters, open wounds).
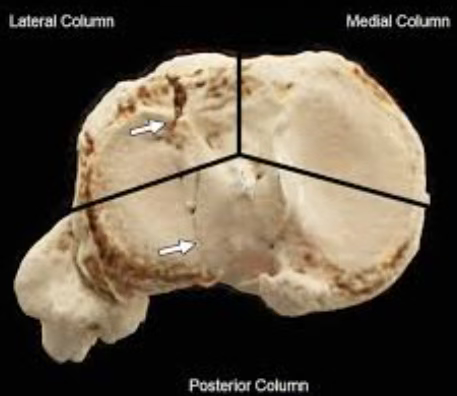
CT is non-negotiable for planning; it reveals posterior column and depression hidden on plain films. Residual step-off >4 mm is a red flag for PTOA and mal-load. Between 2–4 mm lies the “grey zone,” where patient-reported outcomes may match conservative care—so surgery isn’t an automatic win.
Operate or Not: The Decision Tree That Holds Up Under Pressure
Operate when the knee is mechanically unstable, there’s major articular deformation, or soft-tissue threats demand staged fixation. Conserve when displacement is minimal and the knee is stable under stress. Practical rules:
- Absolute ORIF: open fractures, compartment syndrome, neurovascular injury, marked laxity under stress, Schatzker IV–VI.
- Relative: Schatzker I–III with step-off ≥4 mm or clear widening.
- Conservative first: stable patterns with ≤2–3 mm step-off and symmetric valgus/varus stability.
For authoritative background on indications and techniques, see the AAOS OrthoInfo overview on tibial plateau fractures (authoritative clinical resource): AAOS – Tibial Plateau Fractures.
Conservative Pathway: Stage-Based Loading Without Losing Motion
Goal: protect the joint surface while preventing arthrofibrosis. The art is strict axial protection with immediate ROM.
Phase I (0–8 wks):
- NWB with hinged brace; CPM or guided passive/active-assist ROM day 1.
- X-ray surveillance weekly for 3 weeks, then bi-weekly. Target 90° flexion by week 4.
- Priorities: edema control, quad sets, SLRs.
Phase II (8–12 wks):
- Introduce TTWB → PWB: 25% body weight, then +25% each 1–2 weeks.
- Begin closed-chain drills, gait normalization, controlled squats.
Phase III (≥12 wks):
- FWB when radiographs confirm bridging callus; advance to single-leg work, cycling, and balance.
- Expect full functional return at 16–20+ wks.
This cadence guards the surface yet avoids the stiff-knee trap. And yes, it respects tibial plateau fracture weight-bearing timing as a sliding scale, not a stopwatch.
ORIF Pathway: From Traditional Caution to Evidence-Backed Early Loading
Locking plates changed the math. They resist axial load and allow controlled micromotion that fuels osteogenesis. Two paradigms exist:
Traditional (still valid when fixation is tenuous):
- 0–6 wks: NWB/TTWB, immediate ROM.
- 6–12 wks: PWB → FWB by 10–12 wks.
- 12+ wks: higher-level strengthening.
Early FWBAT (when fixation is robust and pattern is simple—often Schatzker I–III):
- Immediate FWB as tolerated with crutches; aggressive ROM from day 1.
- No higher collapse rates in several series; newer RCTs show better pain, gait, and ROM at 6 months versus delay, with similar radiographic integrity.
Clinical filter: early loading only if intra-op reduction is anatomic, locking construct is stout, and bone quality is decent. Otherwise, default to the conservative cadence above. This is still tibial plateau fracture weight-bearing timing—personalized, not permissive.
Patient Selection: The Three Checks That Stop Complications
Before green-lighting load, confirm:
- Fixation stability (intra-op feel + immediate postop films).
- Pattern risk (bicondylar, metaphyseal-diaphyseal dissociation, osteoporotic bone → slower ramp).
- Soft-tissue recovery (no wound compromise).
Red flags to pause or dial back: escalating pain at the plateau, persistent effusion, or any interval depression on radiographs. Pull back 10–15% BW and reassess in 7–10 days—don’t “push through.” A tiny bit of prudence avoids a big revision.
Outcomes, Risks, and the Long Game (PTOA Still Matters)
For minimally displaced, stable fractures, non-operative care often equals surgical function with lower complications and far fewer reoperations (many ORIF reops are symptomatic hardware removals). For unstable/complex injuries, ORIF wins on alignment and stability, yet perfect x-rays don’t immunize against post-traumatic osteoarthritis. The initial chondral insult plus inflammatory storm can seed PTOA even after textbook reduction. Set expectations early: recovery is 6–12 months, and a small fraction will need TKA down the road.
Practical Protocols You Can Print (or Screenshot)
Conservative (stable I–III):
- Weeks 0–8: NWB, brace, immediate ROM → 90° by week 4.
- Weeks 8–12: 25% → 50% → 75% BW, closed-chain drills.
- ≥12 weeks: FWB with strengthening and balance.
ORIF—Traditional (tenuous constructs; V–VI; poor bone):
- Weeks 0–6: NWB/TTWB, ROM.
- Weeks 6–12: PWB → FWB by 10–12.
- ≥12 weeks: power, proprioception, sport-specific.
ORIF—Early FWBAT (stable construct; I–III; good bone):
- Day 0: FWBAT with aids, aggressive ROM, frequent checks.
- Week 2: gait normalization; wean crutches as tolerated.
- Weeks 6–8: higher-level closed-chain, cycling; maintain symmetry.
These flows encode tibial plateau fracture weight-bearing timing for real clinics—not just textbooks.
Counseling That Builds Trust (and Compliance)
Be blunt and humane. Explain that a tibial plateau fracture is a serious intra-articular injury, not a simple “shin break.” Recovery is long; some high-impact goals may be limited. Stress the non-negotiables: follow-up imaging, brace and crutch discipline, and progressive loading guardrails. Small lapses (or bravado) cause big problems.
Bottom Line: Precision Beats Posture
The era of default 12-week NWB is fading. With modern fixation and smarter protocols, early, criterion-based loading can be safe—when the construct and pattern say yes. Let imaging, stability, and soft-tissue reality—not habit—set the pace of tibial plateau fracture weight-bearing timing.
References & Further Reading
- AAOS OrthoInfo: Tibial Plateau Fractures – patient-friendly, clinician-vetted overview of diagnosis and treatment basics: https://orthoinfo.aaos.org/
- Contemporary reviews and RCTs on early loading after ORIF (lock-plate constructs) support criterion-based FWBAT in select Schatzker I–III patterns.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!
More product information:
https://linktr.ee/shifreeman?utm_source=linktree_profile_share<sid=37063a59-a487-42b3-a111-490374634b24




