Supracondylar femur fractures present unique challenges for orthopedic surgeons, particularly in the context of an aging population and increasingly active lifestyles. This article will delve into the pitfalls and danger points associated with these fractures, arming young orthopedic surgeons with the knowledge needed to avoid complications and achieve optimal patient outcomes.
Understanding the Complexity
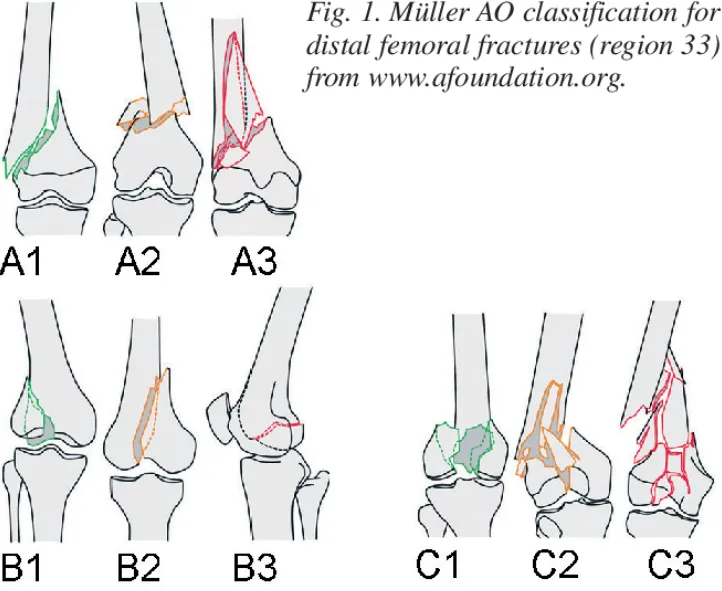
Supracondylar femur fractures are fractures occurring in the distal femur just above the knee joint. They often result from high-energy trauma in younger individuals and low-energy falls in the elderly with osteoporotic bone. These fractures can be complex, involving articular surfaces, significant comminution, and soft tissue injuries.
Missed Associated Injuries: A Critical First Step
A thorough initial assessment is crucial. Always remember that supracondylar femur fractures seldom occur in isolation. Be vigilant for:
· Femoral neck fractures: These can be subtle and easily missed. A high index of suspicion is warranted, especially in elderly patients.
· Patellar fractures: Direct trauma or forceful quadriceps contraction can lead to patellar fractures.
· Tibial plateau fractures: Axial loading forces can transmit to the tibia, causing plateau fractures.
Missing any of these associated injuries can lead to inadequate treatment, prolonged pain, and functional limitations. Employ a systematic examination, supplemented by appropriate imaging studies (X-rays, CT scan) to ensure no injury is overlooked.
The Looming Threat of Vascular Injury
The proximity of the popliteal artery to the distal femur makes it vulnerable to injury. Always assess vascular status meticulously, evaluating for:
· Diminished or absent pulses: Compare the affected limb to the contralateral side.
· Abnormal capillary refill: Delayed refill suggests compromised circulation.
· Sensory changes: Numbness or tingling can indicate nerve compression from a hematoma or direct injury.
· Coolness and pallor: Signs of decreased perfusion.
If vascular compromise is suspected, immediate action is imperative
Obtain a CT angiogram to delineate the injury and consult a vascular surgeon promptly for potential surgical intervention. Delay can lead to irreversible limb ischemia and amputation.

Compartment Syndrome: A Surgical Emergency
Distal femur fractures, especially high-energy injuries, carry a risk of compartment syndrome. Early recognition is essential:
· Pain: Out of proportion to the injury and unrelieved by analgesics.
· Pallor: Pale skin due to decreased blood flow.
· Paresthesia: Numbness or tingling.
· Pulselessness: A late and ominous sign.
· Paralysis: Loss of muscle function, indicating severe ischemia.
Don’t rely solely on one sign. Regularly re-evaluate the patient for these symptoms and maintain a low threshold for measuring compartment pressures.
Prompt fasciotomy is the definitive treatment for compartment syndrome, relieving pressure and restoring blood flow. Delays can result in muscle necrosis, permanent nerve damage, and functional impairment.
Inadequate Articular Reduction: Long-Term Consequences
The articular surface of the distal femur plays a critical role in knee joint function. Failure to achieve anatomical reduction can lead to:
· Post-traumatic arthritis: Joint incongruity accelerates wear and tear, causing pain and stiffness.
· Functional limitations: Malalignment can restrict the range of motion and impair activities like walking, running, and stair climbing.
Precise reduction is paramount Utilize appropriate techniques, including:
· Traction: Gently pulling on the distal fragment to restore length and alignment.
· Joysticks: Instruments that allow controlled manipulation of fragments.
· Clamps: Holding reduced fragments in place before definitive fixation.
Intraoperative fluoroscopy is indispensable for confirming satisfactory reduction.
Retrograde Intramedullary Nailing: Not Without Its Perils
Retrograde intramedullary nailing is a common technique for stabilizing distal femur fractures. However, be mindful of its limitations and potential complications:
· Subtrochanteric Fractures: Retrograde nailing is generally contraindicated, as adequate proximal fixation is difficult to achieve.
· Limited Knee Mobility: Preexisting knee stiffness or limited range of motion can hinder nail insertion.
· Posterior Guidewire Placement: Erroneous guidewire placement and reaming in the posterior intercondylar notch can injure the posterior cruciate ligament.
· Reamer/Nail Impingement: The distal end of the nail must be placed deep to the articular surface to prevent impingement on the patella. Ensure adequate countersinking.
Meticulous surgical technique and careful attention to anatomical landmarks are essential for safe and effective retrograde nailing.
Postoperative Care: A Vital Bridge to Recovery
Postoperative management is equally crucial for optimizing outcomes:
· Early mobilization: Encourage an early range of motion exercises to prevent stiffness and promote circulation.
· Weight-bearing precautions: Follow weight-bearing restrictions as determined by fracture stability and fixation construct.
· Pain management: Provide adequate pain control to facilitate early mobilization and rehabilitation.
· Regular follow-up: Monitor healing progress with radiographs, assess for complications, and adjust the treatment plan as needed.
Conclusion
Supracondylar femur fractures demand a nuanced approach, combining thorough assessment, meticulous surgical technique, and attentive postoperative care. By understanding the potential pitfalls and danger points outlined in this article, young orthopedic surgeons can confidently navigate the complexities of these fractures, minimizing complications, and maximizing patient outcomes.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




