When it comes to displaced pediatric radial neck fractures, percutaneous reduction techniques are often the next step after failed closed reduction. These minimally invasive procedures offer a way to realign the fracture without resorting to more invasive surgery. But when exactly are these techniques indicated, and what methods are commonly used?
Indications for Percutaneous Reduction
The primary indication for percutaneous reduction is the failure of closed reduction after a limited number of attempts. Trying to force a closed reduction repeatedly can cause more harm than good, increasing the risk of complications like vascular injury, nerve damage, or further displacement.
- Key Indications:
- Failed closed reduction after a few attempts.
- Severe displacement that can’t be managed conservatively.
- Avoiding open surgery when possible.
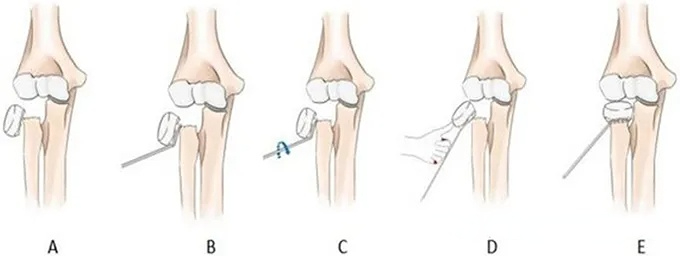
K-Wire Joystick Technique
One of the most commonly used methods is the K-wire joystick technique. In this approach, a K-wire is inserted into the radial neck and used as a lever to manipulate the bone into the correct position. This method allows for precise control and is particularly useful when the fracture is significantly displaced but still reducible percutaneously.
- Advantages:
- Minimally invasive.
- Provides direct control over bone alignment.
- Reduces the need for open surgery.
Leverage Technique
The leverage technique is another effective method. Here, a pin is inserted directly into the fracture site and used as a lever to push the bone back into alignment. This technique is often employed when the fracture is difficult to manipulate with external methods alone.
- Key Points:
- Pin insertion at the fracture site.
- Used to lever the bone into place.
- Effective in severe displacements.
Push Technique
In the push technique, the blunt end of a large K-wire is pressed against the posterolateral aspect of the radial head, pushing it back into position. This method is particularly useful when the fracture displacement is primarily lateral and can be corrected with direct pressure.
- Key Points:
- Blunt K-wire used for direct pressure.
- Ideal for lateral displacements.
- Minimizes the need for open reduction.
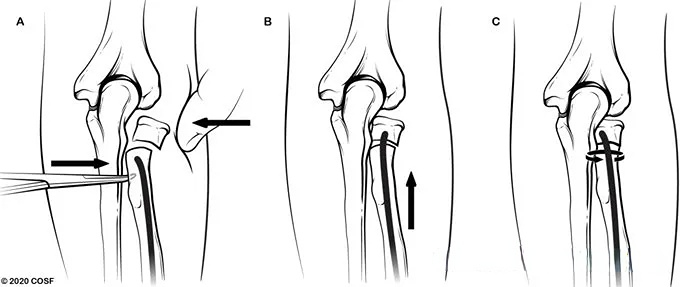
Metaizeau Technique
The Metaizeau technique is one of the more innovative approaches to pediatric radial neck fractures. In this method, a flexible nail is inserted from the distal radius into the intramedullary canal of the bone. The tip of the nail is advanced to the fracture site and into the radial head. By rotating the nail, the surgeon can rotate the radial head back onto the shaft of the bone.
This technique is particularly beneficial for younger patients with significant remodeling potential and helps avoid the complications associated with more invasive procedures.
- Key Points:
- Flexible nail inserted into the intramedullary canal.
- Nail is rotated to align the radial head.
- Effective for younger patients with good remodeling capacity.
Conclusion: Choosing the Right Technique
When closed reduction fails, percutaneous reduction techniques offer a powerful alternative for managing displaced pediatric radial neck fractures. From the K-wire joystick technique to the Metaizeau technique, these methods provide a way to realign the bone with minimal invasiveness. The choice of technique depends on the nature of the fracture and the patient’s age, but all of these methods aim to avoid the need for more invasive surgery. For more detailed information on pediatric fracture management, visit OrthoInfo.
Meta Description:
Discover the most effective percutaneous reduction techniques for displaced pediatric radial neck fractures, including the K-wire joystick, leverage, push, and Metaizeau techniques.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




