Meta Description:
Learn whether suturing the peroneal tendon sheath to the calcaneal plate offers superior stability in calcaneal fracture with peroneal tendon instability, how the technique works, its risks, its clinical outcomes, and when surgeons should consider this innovative approach.
(PAS Hook – Problem / Agitation / Solution)
When surgeons encounter a calcaneal fracture with peroneal tendon instability, the real danger often lies beneath the surface—silent, invisible, and easily overlooked. Nearly half of peroneal tendon instabilities (PTI) are missed at the time of injury, leading to chronic pain, lateral ankle weakness, and tendon degeneration. Even with flawless ORIF, untreated PTI can sabotage outcomes, cause persistent instability, and push patients into long-term dysfunction. This creates a frustrating paradox: perfect bony work ruined by soft-tissue chaos.
But an emerging technique—suturing the peroneal tendon sheath to the calcaneal plate—may offer a direct, stable, and anatomically favorable solution.
(Featured Snippet Answer – Direct, Serious, Helpful)
Yes. Suturing the peroneal tendon sheath to the calcaneal plate appears to be a promising technique for stabilizing the peroneal tendons in patients with calcaneal fracture with peroneal tendon instability. Unlike traditional SPR repair or bone-tunnel fixation, this method anchors only the tendon sheath—not the tendon itself—to the calcaneal plate. This preserves tendon glide, avoids compression, and replicates native restraint without over-constraint. Clinical comparisons show no statistically significant differences in pain, AOFAS scores, FFI, or functional testing versus standard ORIF cases without PTI. Early findings suggest the technique is safe, biomechanically plausible, and may reduce the risk of persistent dislocation. However, a slightly higher rate of sural nerve symptoms was observed, and long-term outcomes require further study. Overall, the technique is a rational option when PTI is discovered intraoperatively through the ELA approach.
(Ref: https://pubmed.ncbi.nlm.nih.gov/)
(Retainer Paragraph – Short, Enticing, Transitional)
The concept is simple. The execution is elegant. And the implications for foot & ankle surgery are significant. If you treat calcaneal fractures, keep reading—this technique challenges old assumptions and may change surgical routines.

Q&A Section: Expert Answers to the Most Critical Questions
1. What is peroneal tendon instability (PTI)?
PTI occurs when the peroneal tendons—normally secured within the retrofibular groove beneath the superior peroneal retinaculum (SPR)—dislocate or subluxate. In calcaneal fracture with peroneal tendon instability, lateral wall blowout or SPR disruption allows the tendons to shift anteriorly over the fibula. Untreated, PTI leads to tendinosis, weakness, chronic pain, and mechanical ankle instability. The instability may involve a torn SPR, bony avulsion, or soft-tissue attenuation.
2. Why is PTI often missed in calcaneal fractures?
Up to 53% of PTI cases are initially misdiagnosed. CT scans only detect bony avulsions; soft-tissue SPR tears without bone fragments are frequently invisible. Soft-tissue swelling masks instability, and the focus on fracture reduction distracts from subtle tendon pathology. Even imaging “normality” does not exclude functional instability—intraoperative SPR testing remains the diagnostic gold standard.
3. How does this new technique differ from traditional SPR repair?
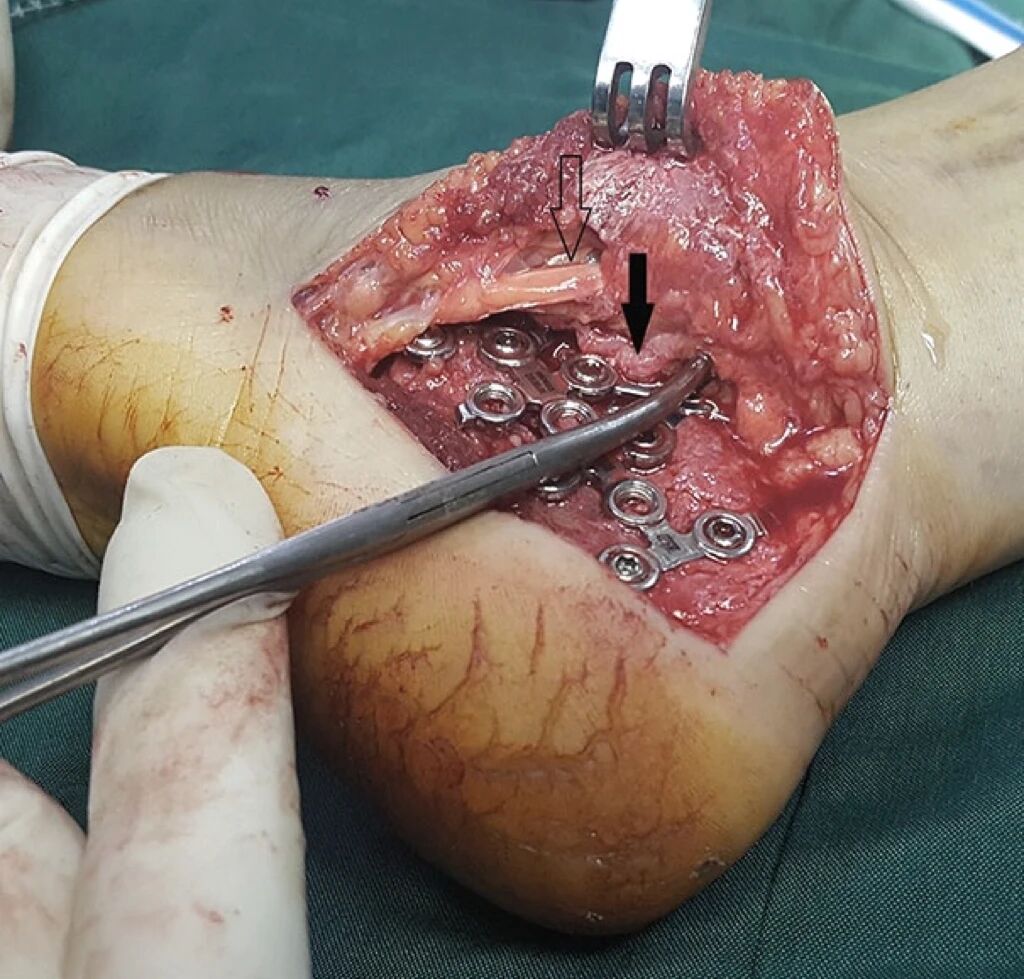
Traditional repair requires an additional posterior incision, direct SPR repair with anchors, or bone-tunnel suture fixation. In contrast, sheath-to-plate fixation uses the existing ELA exposure. Surgeons pass nonabsorbable sutures (e.g., Ethibond No. 2) through the peroneal tendon sheath and secure it to the calcaneal plate frame, restoring posterior containment without manipulating or immobilizing the tendons themselves. This minimizes tissue trauma, preserves tendon mobility, and avoids over-tightening—an issue seen in some SPR reconstructions.
4. What complications may arise from this technique?
While overall complication rates remain comparable to standard ORIF, concerns include:
- Sural nerve irritation or neuropraxia
- Possible peroneal tendon adhesions to the plate
- Transient lateral hindfoot swelling
- Local tenderness along the retrofibular region
However, no significant increase in pain scores, functional limitations, or strength deficits has been reported compared with controls.
5. What did the comparative clinical study reveal?
In a matched cohort study of 12 patients with calcaneal fracture with peroneal tendon instability, outcomes were nearly identical to those in ORIF patients without PTI. No statistical differences were observed in:
- VAS pain
- AOFAS hindfoot scores
- FFI percentage
- Tegner activity scale
- Peroneal muscle strength
Although the PTI group showed slightly lower raw scores, the differences were not significant—suggesting the technique is clinically safe and functionally equivalent to standard ORIF.
6. When should surgeons consider sheath-to-plate fixation?
This technique is particularly useful when:
- PTI is identified intraoperatively during ELA
- SPR is torn without a repairable bony fragment
- Surgeons wish to avoid a second incision
- The peroneal tendons remain mobile and healthy
- Avoiding over-tightening is a priority
In short, it fits perfectly into the workflow of ELA-based ORIF.
7. What are the long-term functional outcomes?
Follow-up averaging around 20 months showed:
- No significant loss of peroneal strength
- Stable tendon positioning on exam
- Normalized gait mechanics
- Comparable sports/activity return
- No recurrence of tendon instability
Long-term (>5 years) data are still emerging, but early outcomes are promising and suggest durable stability.
Conclusion
Suturing the peroneal tendon sheath to the calcaneal plate offers a minimally disruptive, anatomically aligned, and biomechanically sound solution for stabilizing the peroneal tendons in calcaneal fracture with peroneal tendon instability. Early evidence supports its safety and effectiveness, making it a compelling option when PTI is discovered intraoperatively.
References:
1.Vosoughi AR, Hashemipour B, Sahar Khademi, Akbarzadeh A, Shayan Z. Clinical outcomes following suturing of sheath of peroneal tendons to the calcaneal plate as an innovative technique for reduction of peroneal tendon instability accompanying calcaneal fracture. Foot Ankle Spec 2025;18:64–73.
2. Humphrey J, Woods A, Robinson A. The epidemiology and trends in the surgical management of calcaneal fractures in England between 2000 and 2017. Bone Joint J. 2019;101:140-146.Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!
More info. https://linktr.ee/shifreeman




