Operative Correction of Proximal Humerus Varus and Retroversion Deformity in an Adolescent
HSS is the #1 orthopedic hospital in the world. This content was created by our physicians and experts.
ByPeter D. Fabricant, MD, MPH; Nicolas Pascual-Leone, BA; Samuel A. Taylor, MD
FromGrand Rounds from HSS: Management of Complex Cases | Volume 11, Issue 1
Case Report
A 16-year-old boy presented with chronic left shoulder pain, disability, and limited range of motion (ROM). At age 5, he underwent left proximal humerus unicameral bone cyst (UBC) resection, resulting in physeal injury and a complex humeral deformity.
Physical examination (Fig. 1) was notable for left humeral shortening, anterolateral bowing deformity, and 155° of external rotation (ER) compared with 80° on the contralateral side. Internal rotation (IR) was to the coccyx on the left and mid-scapula on the right. The patient reported discomfort and apprehension with terminal ER. Shoulder abduction strength was 4+ on the left and 5 on the right. Preoperative imaging (Fig. 2) demonstrated varus, procurvatum, proximal humeral retroversion, and shortening deformities. Computed tomography scanning revealed a 62° humeral varus deformity, with 41° coming from the humeral diaphyseal bow and 21° from the proximal humerus.
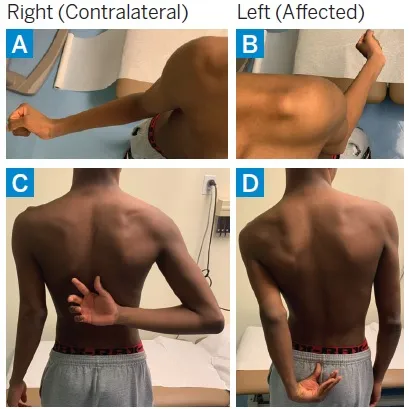
Figure 1:Preoperative physical examination revealed shoulder ER of 80° on the right (a) and 155° on the left (b); IR was to the inferior border of the scapula on the right (c) and to the coccyx on the left (d); the left humerus had 5 cm of clinical shortening.
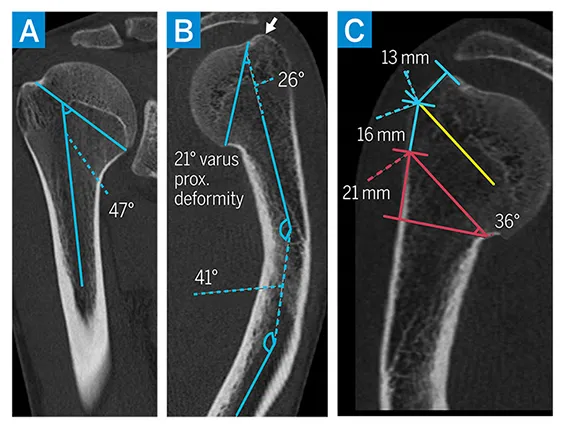
Figure 2:Preoperative CT scan. Compared to the unaffected right side (a), the left side (b) showed 62° of total varus deformity (21° from the proximal humerus), with elevation of the greater tuberosity above the articular margin (arrow). Preoperative planning for proximal humerus deformity correction (c) included an osteotomy that would provide 36° of valgus, 50° of IR, and 15° of forward flexion, with transfer of the long head biceps tendon to the conjoint tendon in order to prevent iatrogenic entrapment.
After several years of failed nonoperative management and functional interference with activities of daily living, the patient was interested in surgical treatment. We performed a multiplanar proximal humerus osteotomy with blade plate and long head biceps tendon transfer using a technique we have reported previously (Fig. 3) [1]. We achieved 36° of valgus correction and 50° of IR correction.
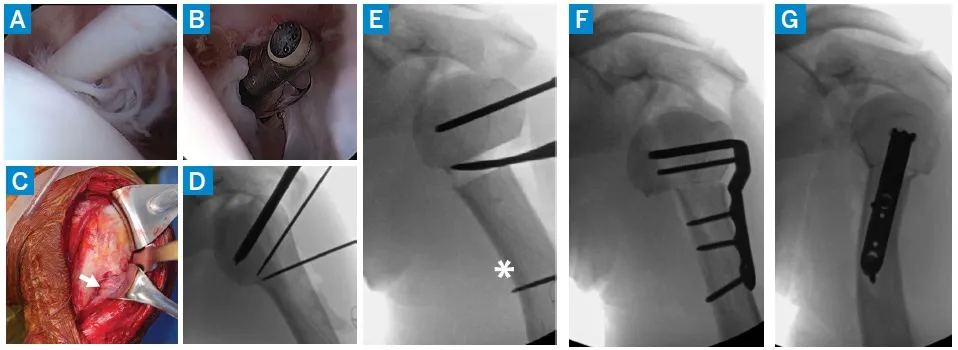
Figure 3: Intraoperative arthroscopy revealed marked long head biceps tendon degeneration at the proximal aspect of the biceps tunnel (a). Biceps tenotomy (b) and an extensile deltopectoral approach to the proximal humerus (c) were performed; the axillary nerve on the undersurface of the deltoid (arrow) was encased in subdeltoid bursal scar tissue. The biceps tendon was then mobilized from the biceps tunnel and tenodesis was performed to the conjoint tendon with nonabsorbable sutures. Guidewires were placed and the proximal fixation chisel for the 90° blade plate (d), closing wedge osteotomy (to assist with rotation deformity correction, an additional guidewire was placed distal to the osteotomy site [asterisk]) (e), and final fixation as seen on AP (f) and lateral (g) fluoroscopy.
At his 6-month visit, the patient demonstrated complete radiographic healing of his osteotomy (Fig. 4 ) and regained maximal ROM (Fig. 5 ), including symmetric ER (80°), IR to mid-scapula, and improved forward flexion. At his 1-year postoperative follow-up, he had resumed full unrestricted activities for 6 months and reported no pain or limitations. He was offered a diaphyseal osteotomy with lengthening to address the residual bowing and length deformity but declined because he had no limitations.
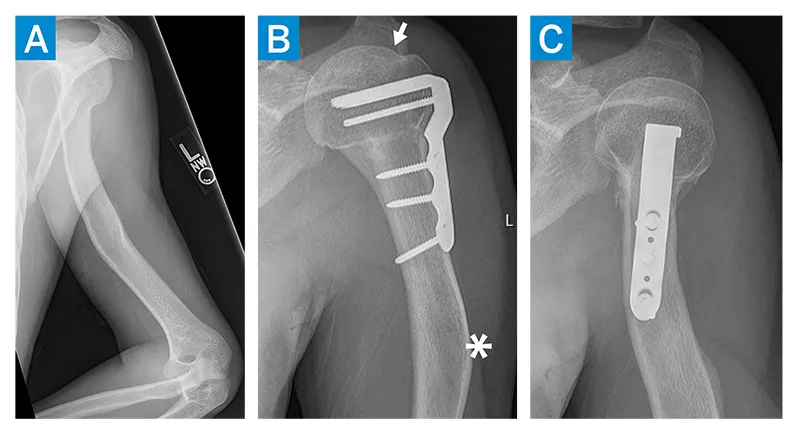
Figure 4: Preoperative radiograph (a) showing a complex multiapical deformity of the left humerus, with proximal humerus varus and ER and extension bowing deformities at the diaphysis. AP (b) and IR (c) radiographs at 6 months postoperative reveal a healed osteotomy, with restoration of the normal proximal humeral geometry. The articular margin was now proximal to the greater tuberosity (arrow), with residual bowing deformity of the shaft (asterisk).
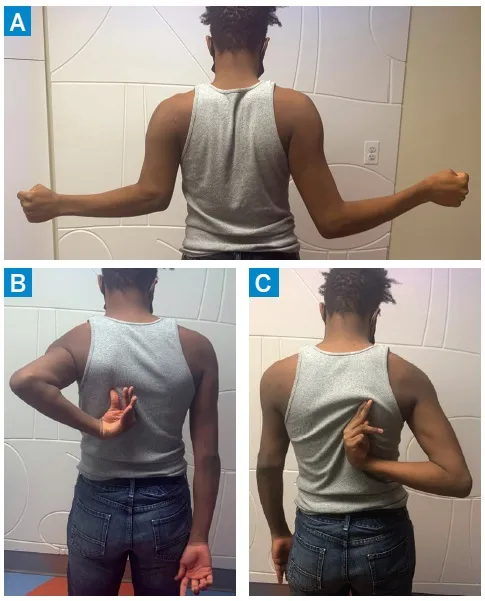
Figure 5: At the 6-month postoperative visit (a) ER was 80° bilaterally. IR was to the scapular body on the left (b) and right (c). There was 6 cm of shortening of the left humerus (compared to 5 cm preoperatively, as noted in Fig. 1).
Discussion
Nonoperative treatment of proximal humerus fractures is typically justified by the remodeling potential in pediatric patients, but persistent deformities can impair shoulder motion through development [2]. Deformities typically arise from congenital, idiopathic, traumatic, hematologic, or infectious etiologies, particularly when there is marked rotational or varus deformity [3]. In this case, the complex humeral deformity resulted from an asymmetric physeal arrest from a proximal humerus UBC resection 11 years earlier. We have used this technique for surgical correction of patients with significant proximal humerus deformities, regardless of cause, whose pain and dysfunction have not responded to nonoperative treatment.
Other authors have described the use of tension band fixation or plate and screw construct [3,4]. Our blade plate technique provides excellent compression andfixation, as well as maximal control of the humeral head fragment for dialing in precise correction. This technique also inhibits further varus deformity in skeletally immature patients by preventing recurrence of asymmetric physeal growth [1].
Posted: 2/18/2022
Authors
Peter D. Fabricant, MD, MPH
Associate Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Scientist, Research Division, Hospital for Special Surgery
Nicolas Pascual-Leone, BA
Research Assistant
Pediatric Orthopaedics
Samuel A. Taylor, MD
Assistant Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopaedic Surgery, Weill Cornell Medical College




