Meta Description:
Hip fractures in the elderly are not just orthopedic injuries — they are systemic emergencies. Learn about postoperative complication management, prevention bundles, and treatment strategies that can reduce mortality and improve recovery outcomes.

Why Hip Fractures Are Called “The Last Fracture of Life”
A hip fracture in older adults is not a bone problem — it’s a life-threatening systemic event. Studies show that up to 75% of patients develop at least one postoperative complication, ranging from delirium and VTE to prosthetic joint infection (PJI).
The fracture itself may heal, but the cascade of complications can lead to permanent disability or death. This is why modern orthopedics demands more than perfect fixation — it demands multidisciplinary vigilance and systemic prevention.
A Full Picture: Systemic vs Surgical Complications
A. Systemic (Internal Medicine) Complications
- Postoperative Delirium (POD): Occurs in 13.5–33% of elderly hip fracture patients. It’s a red flag — often signaling infection, pain, or metabolic imbalance.
- Cardiopulmonary Complications: Heart failure and myocardial ischemia affect up to 40% of cases; pneumonia (7–10%) remains a major killer.
- Venous Thromboembolism (VTE): Even with prophylaxis, DVT/PE occurs in 2–3% of cases within 30 days.
- Urinary Tract Infection (UTI): Common (12–61%) and strongly linked to catheter duration.
- Acute Kidney Injury (AKI): 11% incidence, tied to blood loss, hypotension, and dehydration.
- Malnutrition & Anemia: Hypoalbuminemia in 70% of cases; anemia in nearly half.
B. Surgical (Local) Complications
- Surgical Site Infection (SSI) and PJI: 1.1–6.7% within a year; deep infections often require revision surgery.
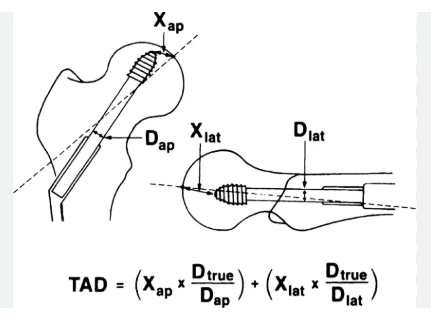
- Implant Failure: “Cutout” occurs in 4–20% of intertrochanteric fractures.
- Nonunion & Avascular Necrosis (AVN): Found in 10–45% and 9–18% of femoral neck fractures respectively.
- Dislocation & Periprosthetic Fracture: Frequent after THA in frail patients.
How to Prevent: Evidence-Based “Prevention Bundle” Approach
A. System-Level Prevention
- Orthogeriatric Co-Management: Joint management by orthopedic and geriatric teams is now the AAOS gold standard. It lowers mortality, delirium, and medical complications through early optimization of comorbidities.
- Surgical Timing (<48 Hours): Not too early, not too late. Surgery within 48 hours — after correction of heart failure, infection, or electrolyte imbalance — is the optimal survival window.
- Anesthesia Strategy:
- ASA II–III: General or spinal anesthesia both acceptable.
- ASA IV or renal impairment: Prefer spinal/epidural to reduce AKI risk.
B. Targeted Prevention Strategies
1. VTE Prevention
- LMWH remains the gold standard; DOACs are not recommended for trauma cases.
- Continue prophylaxis 28–35 days post-op.
- Reference: AAOS VTE Guidelines
2. Delirium Prevention
- Non-pharmacologic bundles: optimize sleep, reorient patients, ensure hearing aids/glasses, mobilize early.
- Avoid benzodiazepines and anticholinergics.
- Pain under-treatment increases delirium risk — regional nerve blocks are superior.
3. Infection Prevention
- UTI: Remove catheters within 24h post-op.
- PJI: Administer prophylactic antibiotics 1–2 hours before incision.
- Cemented femoral stems in arthroplasty lower periprosthetic fracture risk.
4. Mechanical Failure Prevention
- Maintain Tip-Apex Distance (TAD) < 25 mm to prevent cutout.
- Achieve anatomical or slight valgus reduction — never varus.
When Complications Strike: Standardized Response Protocols
A. Systemic Complications
- Delirium: Treat the cause, not the symptom — address hypoxia, infection, or pain before sedation.
- VTE: Confirm with Doppler or CTA; escalate from prophylactic to therapeutic LMWH (1 mg/kg q12h) dosing immediately.
B. Surgical Complications
1. Prosthetic Joint Infection (PJI)
- Diagnosis: Follow 2018 MSIS Criteria.
- Major: Sinus tract or two positive cultures.
- Minor (score ≥6): Elevated D-dimer, CRP, WBC, PMN%, etc.
- Treatment:
- Acute infection → DAIR (Debridement, Antibiotics, Implant Retention)
- Chronic or late infection → 1- or 2-stage revision arthroplasty
2. Fixation Failure
- Femoral Neck Failure: Convert to hemi or total hip arthroplasty (THA).
- Intertrochanteric Failure: If cartilage intact → revision fixation; if destroyed → THA.
Special Populations: Beyond the X-Ray
- Cognitive Decline / Dementia: For late-stage dementia patients, hip fracture signals a “sentinel palliative event.” Focus on comfort, not longevity — discuss care goals with family.
- Secondary Prevention: Start bisphosphonates before discharge. Evidence confirms reduced refracture and mortality.
Key Takeaways
- Hip fracture = systemic disease with orthopedic manifestation.
- Prevention starts with co-management and ends with precision in every screw and decision.
- The real measure of surgical success isn’t fixation — it’s survival without complication.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!
More info. https://linktr.ee/shifreeman




