Meta Description:
This article explores the diagnosis and treatment of peroneal tendon subluxation with ATFL tear, including detailed surgical techniques such as peroneal groove deepening, SPR repair, and modified Broström-Gould reconstruction, following the latest SCARE 2023 guidelines.
Understanding the Pathophysiology
Among the most frequent orthopedic emergencies, ankle injuries remain a diagnostic challenge. Peroneal tendon subluxation, often misdiagnosed as a simple ankle sprain, leads to persistent posterolateral pain and instability. Meanwhile, anterior talofibular ligament (ATFL) tears are the most common cause of chronic lateral ankle instability, accounting for nearly 75% of lateral ankle injuries.
In athletes and active adults, both lesions can coexist. Peroneal tendon instability results from superior peroneal retinaculum (SPR) rupture or avulsion, allowing the tendon to dislocate from its fibular groove during dorsiflexion and eversion. When left untreated, this condition progresses to chronic pain and functional impairment.
Clinical Presentation and Diagnostic Approach
Patients typically present with:
- Persistent lateral ankle swelling and tenderness
- Pain aggravated by inversion or eversion
- Positive anterior drawer and peroneal subluxation tests
MRI remains the gold standard for confirming:
- ATFL rupture
- Peroneal tendinitis and subluxation
- Inflammatory changes or SPR tears
Dynamic MRI or ultrasound during dorsiflexion and eversion enhances diagnostic precision by visualizing real-time tendon instability.
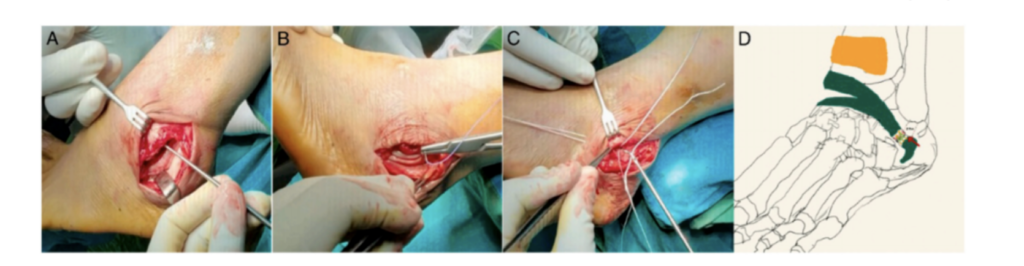
Surgical Technique Overview
The case involves a 47-year-old female patient with peroneal tendon subluxation and ATFL tear, treated through open surgical repair. The operative sequence included:
- Debridement and Tubularization – Removal of degenerated tendon tissue, followed by tubular reshaping for mechanical stability.
- Peroneal Groove Deepening – Using bone flap elevation and cancellous compression to create an 8 mm deepened groove for stable tendon seating.
- SPR Reconstruction – Restoring retinacular continuity to prevent recurrent dislocation.
- Modified Broström-Gould Repair – Anatomical ATFL reconstruction with a 2.9 mm suture anchor, reinforced with the inferior extensor retinaculum.
Postoperatively, pain management was achieved with ketorolac injections, followed by progressive rehabilitation emphasizing ROM, proprioception, and gait training.
Postoperative Rehabilitation and Functional Outcome
A structured three-phase recovery protocol was implemented:
- Weeks 0–2: Non-weight bearing; passive ankle motion within pain tolerance.
- Weeks 3–6: Gradual weight-bearing and proprioceptive training.
- Weeks 7+: Strengthening, agility drills, and single-leg hop testing.
At the 7-week mark, the patient achieved a FADI score improvement from 54 to 101, demonstrating excellent functional recovery with no recurrence or instability.
Discussion: Broström-Gould vs Arthroscopic Techniques
The modified Broström-Gould procedure remains the gold standard for ATFL reconstruction due to its simplicity and high success rate. However, recent studies suggest that arthroscopic Broström-Gould repair offers similar outcomes with:
- Minimal soft tissue trauma
- Faster ROM recovery
- Lower postoperative pain
In this case, open repair was selected due to equipment limitations, yet the results affirm that open techniques remain effective when executed with precision and anatomical restoration.
Clinical Takeaways
- Up to 77% of chronic lateral ankle instability cases involve concomitant peroneal tendon pathology.
- MRI is essential for differentiating subluxation from ligamentous injury.
- Combining groove deepening, SPR repair, and ATFL reconstruction ensures durable stability.
- Postoperative rehabilitation is crucial for restoring proprioception and preventing recurrence.
For further reading, refer to the American Academy of Orthopaedic Surgeons (AAOS) guidelines on ankle instability management.




