Fracture fixation remains one of the most complex areas of orthopedic surgery, demanding precision, technical expertise, and a deep understanding of biomechanics and biology. This article explores the challenges, biological and biomechanical considerations, and optimal treatment strategies for managing fractures, drawing insights from ICUC App case studies and clinical scenarios.
Challenges in Fracture Fixation
Fracture fixation is fraught with complications, ranging from implant failure to delayed healing and infection. Each challenge requires tailored solutions to ensure successful outcomes.
Implant Failure
Internal fixation devices, such as plates and nails, are prone to fatigue, screw breakage, and plastic deformation under excessive load. Multi-fragmentary fractures with insufficient bony support are particularly vulnerable, especially if the fracture fails to consolidate in time.
- Repeated plate failures: A common issue observed in cases like femoral shaft fractures with segmental comminution.
- Non-telescoping implants: These devices bear a high risk of fatigue, making them less suitable for fractures with significant mobility.
Delayed Healing and Non-union
Delayed healing and non-union are frequent complications, particularly after intramedullary nailing.
- Risk factors: Distal fractures, poor reduction, and the use of unreamed nails are strongly correlated with non-union.
- Low strain conditions: Wide fracture gaps stabilized by stiff implants often fail to mechanically induce healing, leading to prolonged recovery times.
Infection
Postoperative infection can devastate fracture fixation outcomes.
- Biofilm formation: Bacteria shielded by biofilms on implants are highly resistant to removal.
- Bone resorption: Infection accelerates bone loss, weakening the fixation site.
- Implant loosening: Tissue reactions to micromotion intensify in infected cases, leading to implant instability.
Technical Errors
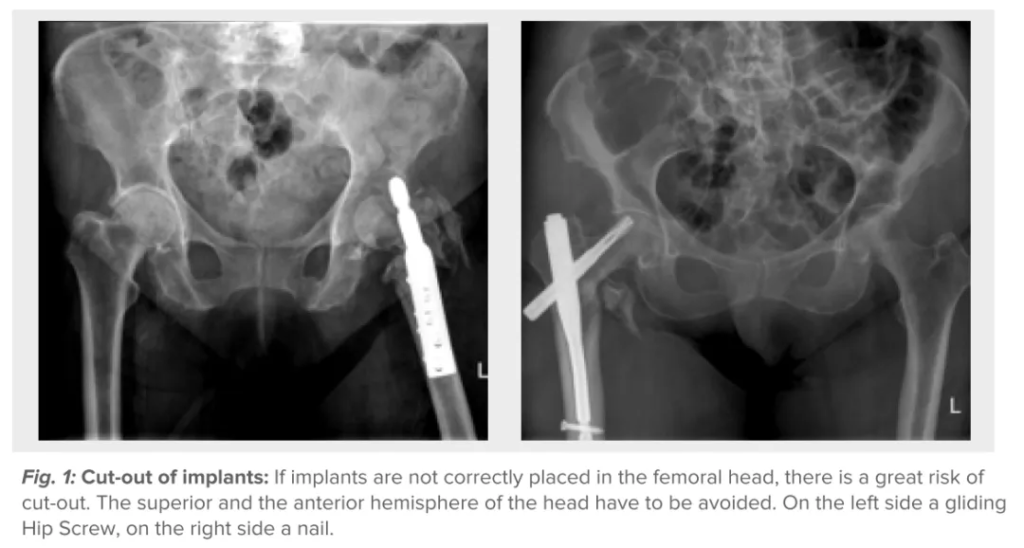
Errors in implant placement, such as incorrect nail entry points or misalignment in the femoral head, can result in cut-out or mal-reduction.
- Rotational instability: Particularly in trochanteric fractures, rotational instability of fragments demands specific anti-rotation devices for correction.
- Poor reduction: Failure to maintain reduction during procedures like nailing exacerbates complications and worsens outcomes.
Biomechanical and Biological Considerations
Successful fracture fixation hinges on balancing mechanical stability with biological preservation. Understanding these principles is critical for optimizing healing and minimizing complications.
Stability
The term “stability” encompasses both stiffness and strength, which are crucial for fracture management.
- Stiffness: Refers to the construct’s resistance to movement under load, influencing strain at the fracture site.
- Strength: Measures the construct’s ability to resist failure under load.
Adequate stability is essential for infection resistance and anatomically correct healing. However, excessive stiffness can hinder callus formation, while insufficient strength risks implant failure.
Strain
Mechanical strain at the fracture site plays a pivotal role in healing.
- Minimal strain: Occurs in wide gaps stabilized by stiff implants, leading to poor mechanical induction of healing.
- Excessive strain: High movement in small gaps can prevent solid bridging and delay recovery.
Adjusting weight-bearing protocols can help optimize strain levels, promoting effective callus formation.
Blood Supply
Preserving blood supply is a cornerstone of fracture healing and infection resistance.
- Surgical techniques: Procedures like periosteal stripping and implant contact can impair blood flow, delaying recovery.
- Elevated plates: Minimizing bone contact through elevated plate designs helps maintain blood supply and reduce complications.
Treatment Options and Techniques
Tailoring treatment strategies to the specific fracture type and clinical scenario is vital for achieving optimal outcomes. Below are some key approaches.
Helical Plate Fixation
The helical plate, a slightly twisted straight plate, is a versatile solution for complex fractures like segmental comminution or defects.
- Advantages: Adds stiffness and strength to the construct while preserving blood supply.
- Minimally invasive: Can be introduced with minimal soft tissue damage, reducing surgical trauma.
- Clinical success: Proven effective after conventional plate failures, allowing immediate pain-free weight-bearing.
Managing Delayed Healing and Non-union
Several strategies can address delayed healing or non-union after nailing:
- Exchange nailing: Standard for short oblique isthmal fractures, often involving reaming to stimulate healing.
- Plate augmentation: Adding a plate alongside the existing nail is an alternative, particularly for complex fracture patterns. This can be performed minimally invasively.
- Dynamization: Removing locking screws to allow controlled movement remains controversial and biomechanically challenging to justify.
Managing Trochanteric Fractures
Trochanteric fractures require a deep understanding of fracture patterns and precise techniques:
- Cerclage wires/cables: Improve and maintain reduction while addressing rotational instability.
- Anti-rotation devices: Preferably placed through a buttress plate for enhanced stability.
- Blade plates: Useful for revision cases with technical challenges.
Overcoming Complications
Despite advancements in fracture fixation, complications like infection, implant loosening, and screw stripping persist. Effective management strategies include:
- Stable fixation: Essential for minimizing micromotion and preventing infection.
- Biotolerant materials: Titanium implants offer superior tissue tolerance compared to stainless steel, particularly in infected cases.
- Biofilm management: Suspected biofilm formation may necessitate implant replacement.
Assessing Healing
Accurate assessment of fracture healing is crucial for guiding treatment decisions.
- Conventional X-rays: Often insufficient for evaluating fracture gaps or bone contact.
- CT scans: Provide detailed insights into healing progress, especially in complex cases.
Careful review of CT slices is mandatory for determining weight-bearing protocols and ensuring proper recovery.
SEO Keywords and Tag
Primary Keywords
- Fracture fixation challenges
- Biomechanical considerations in orthopedic surgery
- Helical plate fixation
Secondary Keywords
- Managing non-union after nailing
- Trochanteric fracture treatment
- Blood supply in fracture healing
Long-Tail Keywords
- Minimally invasive techniques for fracture fixation
- How to handle implant failure in orthopedic surgery
- Biomechanical strain and fracture healing
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




