(PAS Hook — Paragraph 1)
Hip surgeons often assume proximal femoral nail fixation is a beginner-level procedure — quick, routine, almost mechanical. Yet every year, implants cut out, nails penetrate the anterior cortex, elderly patients collapse into varus, and what should have been a straightforward fixation ends in catastrophic failure. The worst complications—cut-out, cut-through, anterior cortical impingement, and iatrogenic fractures—are not accidents of fate. They are predictable. They are preventable. And they originate not from hardware, but from technique. When we approach PFN surgery casually, we fall into traps built into the anatomy, the fracture pattern, the reduction strategy, and even the nail we choose.
(Featured Snippet Section — Formal Answer)
To avoid failure in proximal femoral nail (PFN) fixation, surgeons must master five critical domains: reduction quality, entry point accuracy, anterior cortical curvature awareness, implant selection strategy, and TAD/CalTAD precision. Varus malreduction, rotational mismatch, wedge-effect collapse during nail insertion, anterior cortical impingement from mismatch between nail ROC and femoral bow, and incorrect implant choice (PFNA vs Intertan) drastically increase mechanical failure rates. Proper reduction should prioritize valgus or neutral alignment, a precise entry point at or slightly medial to the greater trochanter apex, Poller pin use in high femoral bow cases, implant decisions based on bone density and fracture type, and strict TAD <25 mm positioning (inferior-center screw trajectory). These actions minimize cut-out, reduce stress concentration, and improve functional recovery.
(Retainer — Smooth Transitional Paragraph)
Simple decisions determine success: where you enter, how you reduce, which implant you choose, and where your screw sits. The operation is easy—until it isn’t. Keep reading, because every pitfall you prevent is a fracture you never have to revise.
Relevant Questions and Detailed Answers
1. Why is varus malreduction the number one enemy in proximal femoral nail fixation?
Because varus alignment (<125°) dramatically increases the risk of cut-out. When the femoral head collapses, the screw migrates superiorly, penetrating the cortex like a blade through soft fruit. Even worse is the subtle wedge effect — the PFN acts like a chisel; if reaming is insufficient or the entry point drifts lateral, the proximal fragment is pushed into varus even after a seemingly perfect reduction. The solution? Aim medial at the apex, perform adequate proximal reaming, and use hollow reamers to remove—rather than compact—bone. Good reduction is not repairable with metal. Nail doesn’t correct mistakes. It amplifies them.
2. How do rotation errors and excessive traction silently sabotage fixation?
On the traction table, gravity externally rotates the leg. Surgeons watch the screen, not the limb — and lose anteversion. The giveaway? Small trochanter sign. If the lesser trochanter looks too prominent, rotation is wrong. High traction separates fragments (>3 mm) and invites non-union. Fix it early: relax traction, back-hammer gently before distal locking, or compress with Intertan. Rotation cannot be fixed post-op. What you accept on table, you accept in radiographs forever.
3. What makes anterior cortical impingement a ticking time bomb?
The human femur curves anteriorly (ROC ≈1200 mm), while many older nails are straighter (1500–2000 mm). A straight nail in a curved canal means the distal tip slams the anterior cortex. Consequences range from anterior thigh pain to late femoral shaft fracture. Prevention strategies demand obsession:
- Use Poller Pin (Steinmann) guidance, placed anteriorly if nail drifts forward
- Choose smaller ROC nails (1.0–1.5 m) in short stature or high curvature femurs
- Short nails exist, but stress concentration risk increases
This is not a small issue — it is one of the main revision triggers globally (see https://pubmed.ncbi.nlm.nih.gov/ for supporting data).
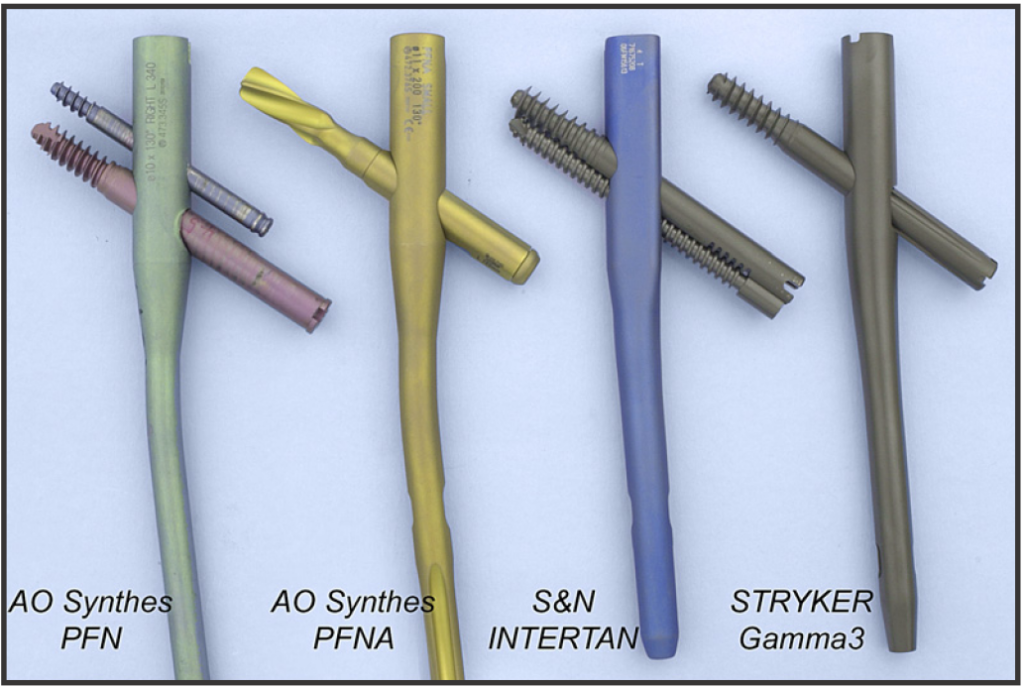
4. PFNA vs Intertan — which implant fails, and why?
Two mechanisms, two disasters:
- PFNA → Cut-through
The helical blade offers superior anti-rotation, but poor axial resistance. In osteoporotic bone, collapse drives the blade inward, and the head swallows the implant. - Intertan → Stability powerhouse
Dual-screw box mechanics lock rotation and resist collapse. Distal fork design lowers stress. Ideal for 31-A3 fractures, younger patients, functional demand cases.
If the patient is fragile, bleeding risk matters, and time is limited → PFNA is forgiving.
If the fracture is unstable, patient is active, and failure is not an option → Intertan wins.
5. How important are TAD and CalTAD — do millimeters really matter?
They are everything. TAD must be <25 mm, full stop. On AP view the screw should kiss the inferior cortex, and on lateral view it must sit center — inferior + central = survival. Superior placement is death zone. Every millimeter upward multiplies cut-out risk. CalTAD adds sensitivity by including inferior AP positioning in its calculation, and surgeons obsessed with CalTAD have fewer revisions.
Final Summary
Master reduction. Respect femoral anatomy. Choose implants purposefully. Aim for TAD <25 mm. Because proximal femoral nail fixation is not an entry-level operation — it is a minefield navigated only by those who understand where the bombs lie.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!
More info. https://linktr.ee/shifreeman




