For decades, Pilon fracture management has been anchored in dogma — staged fixation, fibular reconstruction, standard anterior approaches, and “fusion as last resort.” But recent 2023–2024 studies are rewriting those rules. Here’s a sharp, evidence-based comparison between traditional orthopedics and the modern trauma mindset.
Primary Keywords: Pilon fracture, staged fixation, fibular fixation, ankle fusion
Reference: AAOS Trauma Surgery Updates
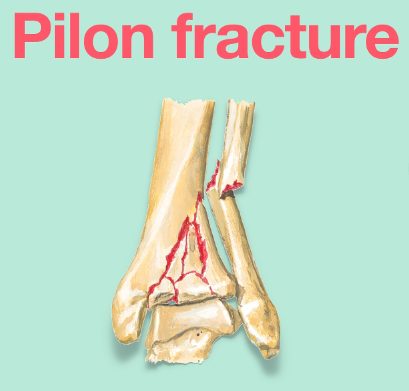
1️⃣ The Myth of “Staged Fixation” as an Absolute Rule
Classic View:
“Two-stage management” — initial external fixation followed by delayed ORIF — was long hailed as the gold standard for Pilon fractures.
Immediate internal fixation was reserved for rare, low-energy, closed fractures with pristine soft tissue. Any deviation was deemed reckless.
Modern View:
Recent prospective studies (2023–2024) challenge this rigidity. For carefully selected cases — low-energy, closed fractures with mild swelling — single-stage internal fixation yields similar infection and nonunion rates, with faster recovery and shorter hospital stays.
🧠 Key Insight:
“Two-stage” remains the rule for high-energy comminuted Pilons, but modern evidence supports individualized decisions based on injury biology and surgeon expertise — not dogma.
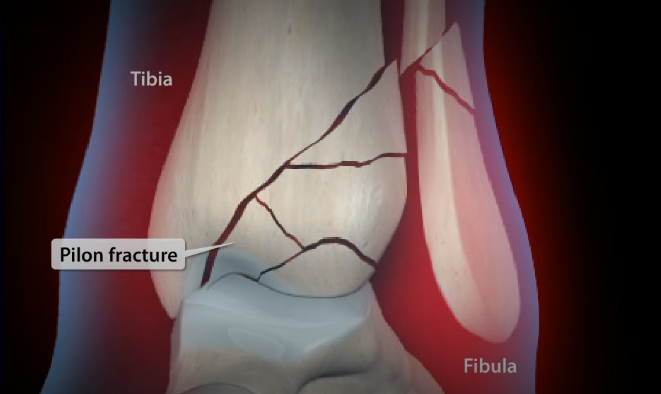
2️⃣ Rethinking Fibular Fixation — Beyond Alignment
Classic View:
Fixing the fibula restores length, rotation, and alignment, indirectly reducing the tibia via ligamentotaxis — a mechanical step before addressing the articular surface.
Modern View:
New 2024 comparative studies reveal a deeper benefit: patients without fibular fixation showed significantly higher rates of post-traumatic arthritis, despite equal union rates.
Thus, fibular fixation isn’t just for mechanical alignment — it’s biological prevention of joint incongruity and arthrosis.
⚙️ Core Shift:
The fibula is not “optional hardware.” It’s the lateral column of long-term joint survival.
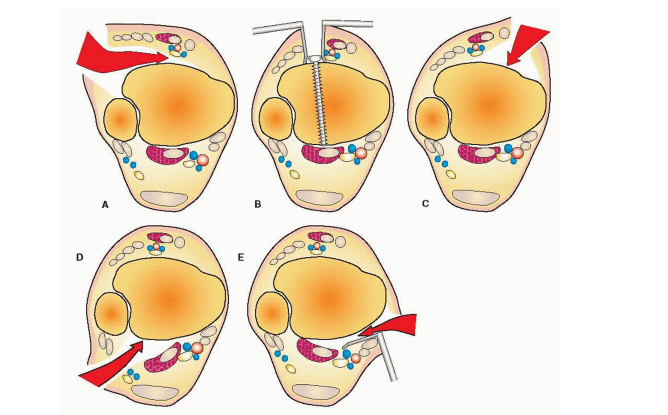
3️⃣ Surgical Approach: From “Exposure” to “Strategy”
Classic View:
Standard approaches — anteromedial, anterolateral, posteromedial, posterolateral — were chosen primarily for what structures they expose.
“Anteromedial” became the default entry point for most Pilon ORIFs.
Modern View:
Two strategic innovations redefine the field:
A. The “Posterior-First” Principle
Fix the posterior column and fibula early (via posterolateral incision), creating a solid base for subsequent anterior reconstruction — a “backbone-first” concept improving articular alignment.
B. The “Direct Anterior (DA) Approach”
Introduced in 2024 studies, this approach anticipates the future: many Pilon fractures will require salvage fusion or total ankle arthroplasty. Using the DA corridor initially preserves a clean plane for future surgery — less scarring, fewer complications, and easier revisions.
💡 Strategic Evolution:
Surgical approach is no longer about “what you can see,” but about how you set the stage for a patient’s entire lifetime of ankle function.
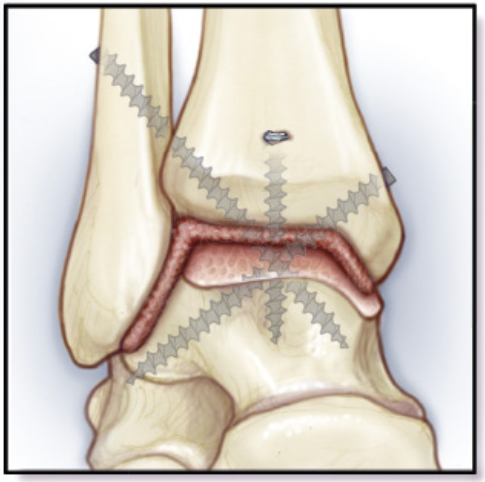
4️⃣ Primary Ankle Fusion: From “Last Resort” to “Smart Start”
Classic View:
Primary ankle fusion was reserved for “hopeless” cases — severe comminution, cartilage loss, chronic infection. Fusion was viewed as failure, trading mobility for stability.
Modern View:
A 2021 systematic review flipped the paradigm:
In severe C3 Pilon fractures, primary fusion showed:
- Lower wound complications: 2.9% vs. 14.6%
- Lower malunion/nonunion: 2.9% vs. 9.9%
- Equal or better functional outcomes vs. staged ORIF
🚀 Takeaway:
In the worst fractures, fusion is not surrender — it’s strategy. Instead of chasing an unsalvageable joint, fusion delivers a stable, pain-free, functional limb with fewer reoperations.
SEO Keywords: primary ankle fusion, Pilon fracture, C3 fracture, complication rate, functional recovery.
🎯 Final Verdict: Knowledge Evolution in Real Time
- Traditional concepts are safe, structured, and fundamental — the language of sound orthopedics.
- Modern perspectives represent critical thinking and personalization — the mindset of a trauma expert.
The shift isn’t rebellion; it’s refinement. Evidence doesn’t erase the “gold standard,” it polishes it.
A modern Pilon fracture surgeon knows both — the rules, and when to break them intelligently.
References:
- AAOS Trauma Updates 2024
- “Contemporary Management of High-Energy Tibial Pilon Fractures” — J Orthop Trauma, 2024
- “Primary Ankle Arthrodesis in C3 Pilon Fractures: A Systematic Review,” Bone & Joint J, 2021
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!
More info. https://linktr.ee/shifreeman




