Humeral shaft fractures are a common orthopedic injury, but not all cases require surgical intervention. Determining when surgery is necessary depends on a combination of clinical, anatomical, and patient-specific factors. In this guide, we’ll break down the absolute and relative indications for surgical treatment of humeral shaft fractures, providing clarity for clinicians and patients alike.
Absolute Indications for Surgery
Certain circumstances make surgical intervention unavoidable. These absolute indications are based on the severity of the injury, associated complications, or the inability to achieve acceptable alignment through non-operative means. Here are the key scenarios where surgery is mandatory:
- Unacceptable alignment by closed means: When closed reduction fails to restore proper alignment, surgery becomes essential.
- Polytrauma: In patients with multiple injuries, stabilizing the humerus surgically can aid in overall recovery and rehabilitation.
- Bilateral humeral shaft fractures: Non-operative management is impractical for both arms, necessitating surgical fixation.
- Floating elbow: A combination of humeral and forearm fractures requires surgical stabilization to restore limb function.
- Intra-articular extension: Fractures involving the shoulder or elbow joint demand precise alignment, achievable only through surgery.
- Vascular injury requiring repair: When blood vessels are compromised, surgical intervention is critical to restore circulation.
- Neurologic deficit after penetrating injury: Surgery may be required to explore and repair nerve damage.
- Nonunion: Failure of the bone to heal after conservative treatment often necessitates surgical correction.
- Pathologic fracture: Fractures caused by underlying conditions like cancer or osteoporosis require stabilization and further evaluation.
- Skin conditions precluding bracing (e.g., burns): When external bracing is not feasible, internal fixation is the only option.
- High-velocity gunshot wounds: These injuries often result in severe bone and soft tissue damage, necessitating surgical intervention.
- Progressive nerve palsy or nerve palsy after closed manipulation: Worsening neurological function following non-operative attempts signals the need for surgery.
Relative Indications for Surgery
While not always mandatory, certain situations make surgical treatment preferable. These relative indications often depend on patient factors, fracture characteristics, or the likelihood of complications with conservative treatment. Surgery may be considered in the following cases:
- Open fractures: While some can be managed non-operatively, many open fractures benefit from surgical stabilization to reduce infection risk and improve healing.
- Segmental fractures: These complex fractures are challenging to manage conservatively and often require surgical fixation.
- Noncompliant patients: Patients unable to adhere to non-operative protocols, such as bracing, are better suited for surgery.
- Obesity or large breasts: Anatomical challenges can make bracing ineffective, necessitating surgical stabilization.
- Periprosthetic fractures: Fractures around an existing implant or prosthesis require surgical management to ensure stability.
- Transverse or oblique middle 1/3 fractures: These fracture patterns are prone to displacement, making surgery a more reliable option.
- Long oblique fracture of the proximal 1/3: The risk of malunion or nonunion is higher in these fractures, favoring surgical intervention.
Why Surgical Treatment Matters
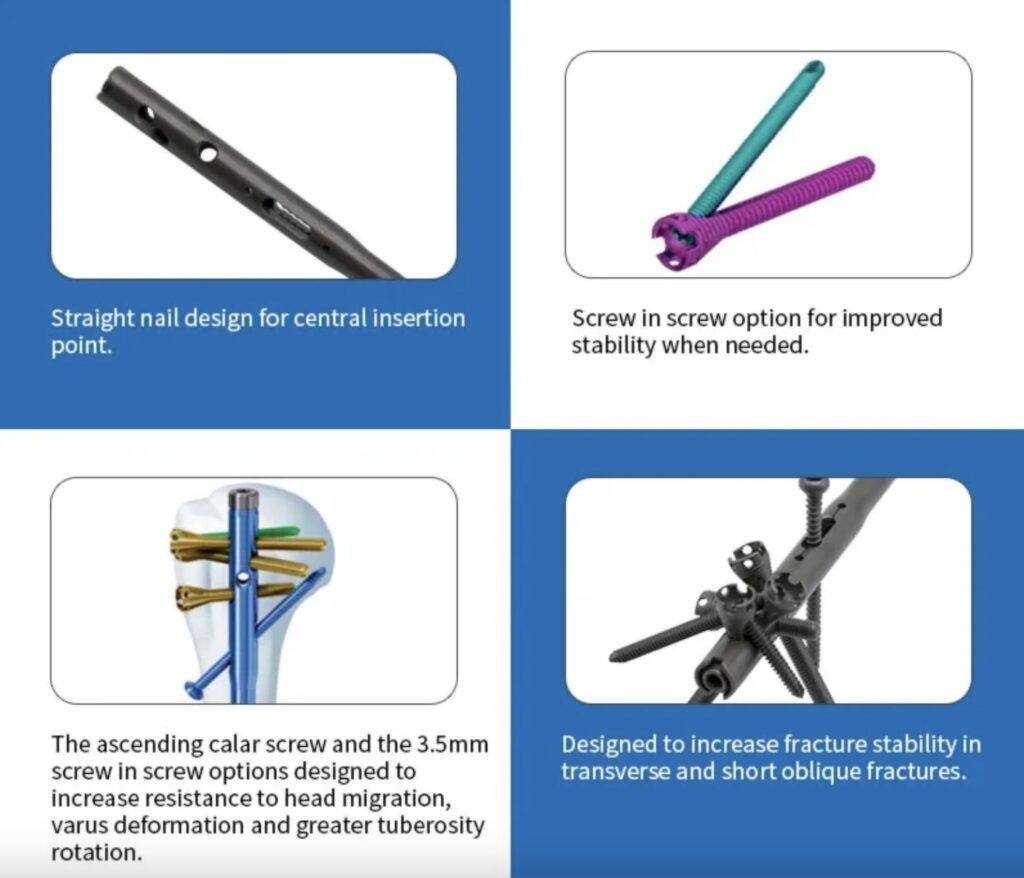
Surgical intervention for humeral shaft fractures is not a one-size-fits-all approach. The decision to operate must consider the patient’s overall health, activity level, and the specific nature of the fracture. Modern surgical techniques, including intramedullary nailing and plate fixation, offer excellent outcomes when applied appropriately.
Advantages of Surgery:
- Faster mobilization and return to daily activities.
- More predictable healing compared to conservative methods.
- Reduced risk of malunion or nonunion.
However, surgery is not without risks, including infection, nerve damage, and potential hardware complications. These risks must be weighed against the benefits on a case-by-case basis.
For a deeper dive into the management of humeral shaft fractures, visit this AAOS resource on fracture care.
Conclusion
Understanding the indications for surgical treatment of humeral shaft fractures is critical for optimizing outcomes. Whether dealing with absolute indications, such as vascular injury or intra-articular extension, or relative factors like patient compliance and fracture pattern, the decision to operate should be guided by evidence-based practices. By tailoring treatment to the individual, clinicians can ensure the best possible recovery for their patients.
Meta Description:
Learn the absolute and relative indications for surgical treatment of humeral shaft fractures. Explore when surgery is essential, from vascular injuries to nonunion, and understand modern approaches to fracture care.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




