Lumbar Spinal Stenosis (LSS) is a progressive degenerative condition that affects millions worldwide, particularly those over the age of 65. With the aging population on the rise, Minimally Invasive Surgical Treatments (MIST) are rapidly advancing, offering safer and more effective options. This article updates the 2019 MIST guidelines, providing a cutting-edge framework for diagnosing and treating lumbar spinal stenosis.
What Is Lumbar Spinal Stenosis (LSS)?
Definition and Classification
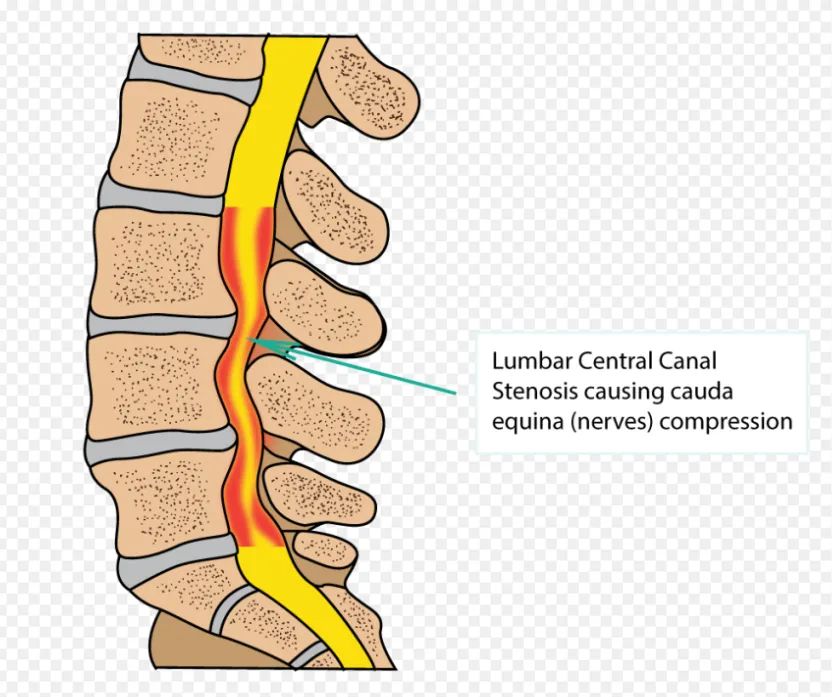
Lumbar Spinal Stenosis (LSS) refers to the narrowing of the spinal canal, lateral recess, or neural foramina, leading to compression of neurovascular structures. This often results in buttock or leg pain, and sometimes lower back pain. LSS can be classified based on the location of the narrowing:
- Central Canal Stenosis: Characterized by a reduced thecal sac diameter (<10mm). Symptoms include neurogenic claudication (NC), where pain worsens with standing or walking and improves with sitting or spinal flexion.
- Lateral Recess Stenosis: Narrowing of the lateral recess (<4mm) that may cause radiculopathy, with or without neurogenic claudication.
- Foraminal Stenosis: Narrowing of the neural foramina, often caused by facet joint hypertrophy or disc herniation, presenting as radicular leg pain and limited lumbar mobility.
- Multistructural Stenosis: Involves narrowing in multiple regions, commonly seen in patients over 60, with symptoms combining the above types.
Symptoms and Diagnosis
Patients with LSS often report neurogenic claudication, which includes leg pain, numbness, or weakness that worsens with standing or walking and improves with sitting or spinal flexion. Imaging studies, such as MRI or CT, are the gold standard for diagnosis, with upright hyperlordotic MRI being particularly sensitive for dynamic stenosis. Differential diagnoses to consider include:
- Peripheral Neuropathies: Distinguished by pain at rest and a length-dependent distribution (e.g., “stocking and glove”).
- Vascular Claudication (VC): Unlike NC, VC pain does not improve with posture changes and is often associated with vascular risk factors.
- Lumbar Radiculopathies: Characterized by dermatomal pain and numbness, which can be localized using the straight leg raise test.
Advances in Minimally Invasive Surgical Treatments (MIST)
1. Percutaneous Image-Guided Lumbar Decompression (PILD)
PILD is a minimally invasive procedure that uses imaging guidance to remove portions of the lamina and ligamentum flavum, relieving nerve compression.
- Indications: Symptomatic LSS with neurogenic claudication confirmed by imaging, with ligamentum flavum hypertrophy ≥2.5mm.
- Contraindications: Prior surgery at the target level, localized infection, or relative contraindications such as spondylolisthesis > grade 2 or bleeding disorders.
Evidence: Level 1 randomized controlled trials (RCTs) demonstrate that PILD is superior to epidural steroid injections (ESI) for treating neurogenic claudication caused by ligamentum flavum hypertrophy, with sustained long-term benefits.
2. Interspinous Spacers
These devices are implanted between spinous processes to limit spinal extension and indirectly decompress the spinal canal.
- Indications: Moderate degenerative LSS with symptoms relieved by spinal flexion and failure of at least 6 months of conservative treatment.
- Contraindications: More than 2 levels of moderate stenosis, severe stenosis, spondylolisthesis > grade 1, osteoporosis, or prior fusion/decompression surgery at the index level.
Evidence: Studies show that interspinous spacers can effectively reduce pain and improve function, though additional high-quality RCTs are needed to confirm long-term outcomes.
3. Open Decompression Surgery
Open decompression is a traditional surgical method involving the removal of bone or soft tissue compressing the neural structures.
- Indications: Degenerative LSS unresponsive to conservative treatment, particularly with progressive neurological deficits.
- Contraindications: Spinal instability or coagulopathy, with relative contraindications including scoliosis, kyphosis, and high-grade spondylolisthesis.
Evidence: Open decompression surgery provides significant pain relief and functional improvement compared to non-surgical management. However, the necessity of concurrent spinal fusion remains a topic of debate.
The MIST 2.0 Treatment Algorithm
The MIST 2.0 Algorithm offers a stepwise approach to LSS treatment, emphasizing the importance of patient-specific characteristics and anatomical variations:
- Conservative Management: Includes physical therapy, oral medications, and injections such as ESI.
- Minimally Invasive Procedures: Options like PILD or interspinous spacers are recommended for moderate LSS.
- Open Surgery: For severe symptoms or cases unresponsive to conservative treatments, open decompression or intrathecal drug delivery systems (IDDS) may be considered.
This algorithm is designed to evolve with emerging evidence. For more information on MIST 2.0, visit the American Academy of Orthopaedic Surgeons (AAOS) guidelines.
Conclusion
The treatment of lumbar spinal stenosis is entering a new era of precision and personalization. By integrating minimally invasive techniques with traditional surgical methods, MIST 2.0 provides a tailored approach to optimize patient outcomes. From PILD and interspinous spacers to open decompression surgery, each method has its unique indications and contraindications. For clinicians, understanding these nuances and aligning treatment with individual patient needs is key to achieving the best results.
Meta Description:
Discover the latest minimally invasive treatments (MIST 2.0) for lumbar spinal stenosis, including PILD, interspinous spacers, and open surgery. Learn about cutting-edge techniques to optimize patient care.
Social media content generation complete. Please input new requirements. Avoid using any invisible spaces that may allow AI detectors to identify the text.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




