Volkmann #fracture, also known as posterior #malleolus fracture, is an avulsion fracture of the posterior tibiofibular ligament at the starting point of the tibia. The fracture fragment may or may not involve the posterior malleolus joint surface. In the original report by German doctor Volkmann in 1875, Volkmann fracture actually described an avulsion fracture of the anterolateral distal tibia in the sagittal plane (but it was accidentally passed down as a fracture of the posterior lateral tubercle of the ankle joint). The posterior malleolus plays an important role in maintaining the stability and function of the ankle joint. Posterior malleolus fractures account for about 7% to 44% of ankle injuries. Studies have shown that when ankle fractures involve the posterior malleolus, the treatment effect is usually unsatisfactory. Poor fracture reduction can lead to complications such as malformation, pain and limited activity. Osteotomy and correction surgery are required for patients with obvious symptoms. Haraguchi et al. divided posterior malleolus fractures into three types: type I, posterior external oblique type; type II, medial extension type; type III, small shell type (small piece peeling type). Mangnus et al. believe that posterior malleolus fractures can be divided into two basic types: posterior external type and posterior medial type. Based on CT scanning and three-dimensional reconstruction, Bartonícek et al. classified posterior malleolus fractures into four types according to factors such as the location, shape, size, and integrity of the tibial notch: type I, extra-notch fracture; type II, posterolateral fracture; type III, two-part posterior malleolus fracture; and type IV, posterolateral large triangular fracture. The morphology of posterior malleolus fractures varies greatly between individuals, and there is currently no universally accepted classification method that can fully reflect the injury mechanism and degree of fracture and provide guidance for treatment. The size of the fracture fragment is still an important factor in determining whether internal fixation is required for posterior malleolus fractures. Patients should have anteroposterior and lateral ankle X-rays taken after injury to understand ankle fractures, dislocations, and ligament injuries. At the same time, CT and three-dimensional reconstruction should be used to conduct detailed preoperative evaluation and planning of the morphology, size, and degree of displacement of the posterior malleolus fracture fragment to determine the appropriate surgical approach, such as the posterolateral approach, posteromedial approach, or a combined posterolateral and posteromedial approach to the ankle joint. Screws or plates should be selected for internal fixation according to the size of the fracture fragment to achieve the anatomical reduction of the posterior malleolus fracture, restore the flatness of the articular surface, and the stability of the tibiotalar joint and the distal tibiofibular syndesmosis.

Bartonícek classification
Lateral #malleolus fracture combined with posterior malleolus fracture can usually be treated with open reduction and fixation of the lateral malleolus and posterior malleolus fracture fragments through the posterolateral approach to the ankle joint. The goals of anatomical reduction of the posterior malleolus fracture fragment are: 1. Reconstruction of the distal tibial articular surface and fibular notch; 2. Restoration of posterior stability of the tibiotalar joint; 3. Reconstruction of the posterior tibiofibular ligament; 4. Reduction of the fibula to the reconstructed fibular notch through reduction of the posterior tibiofibular ligament. This post will introduce the techniques of treating lateral malleolus and posterior malleolus fractures through the posterolateral approach to the ankle joint in a graphic and textual manner.
|Posterolateral approach to the ankle|
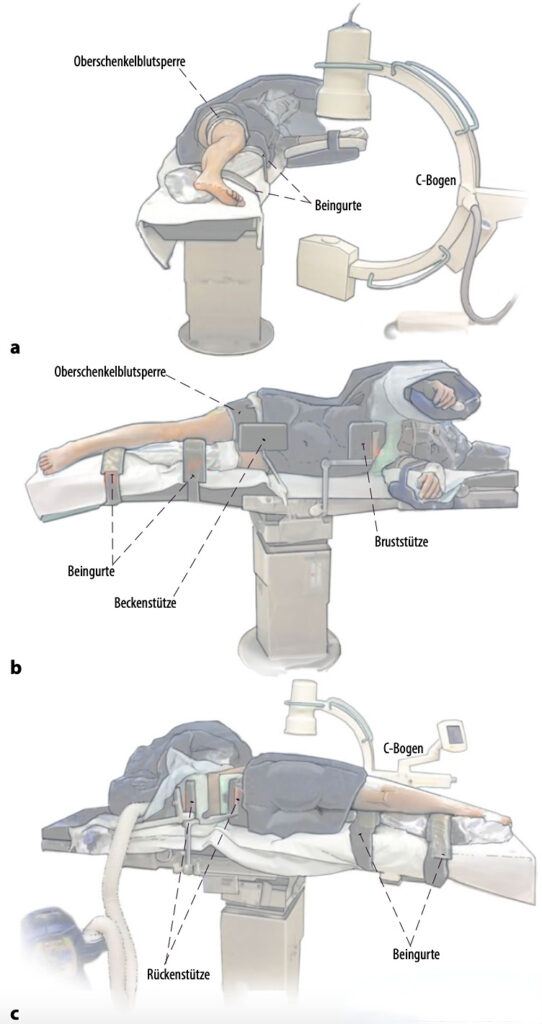
▲The figure shows a schematic diagram of the lateral decubitus position (a). The patient can be transferred to the supine position during surgery by removing the side and back supports (b, c) without the need for disinfection and draping again. The advantage of this position is that it can be used for arthroscopic fracture treatment and treatment of anterior tibiofibular ligament avulsion fractures (Chaput fractures, Wagstaffe fractures) and ligament injuries, or a floating position can be used.

▲The picture shows the patient in the lateral position during surgery, which also shows the position of the C-arm machine and the arthroscopic system.
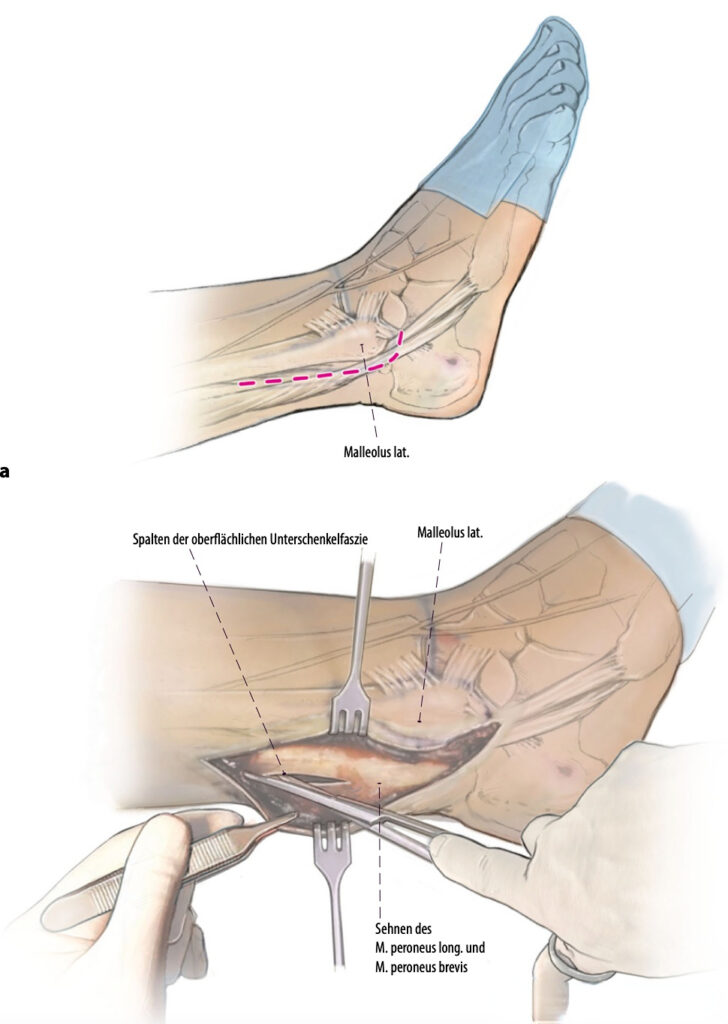
▲The figure shows combined treatment through the posterolateral approach when treating ankle fractures involving the posterior malleolus. Note that the skin incision is to protect the sural nerve. The skin incision should be made directly on the posterior side of the peroneal tendon and bend forward at the tip of the fibula (red dotted line). Directly open the superficial fascia on the posterior side of the fibula. If the peroneal tendon aponeurosis is accidentally opened, it should be sutured last.
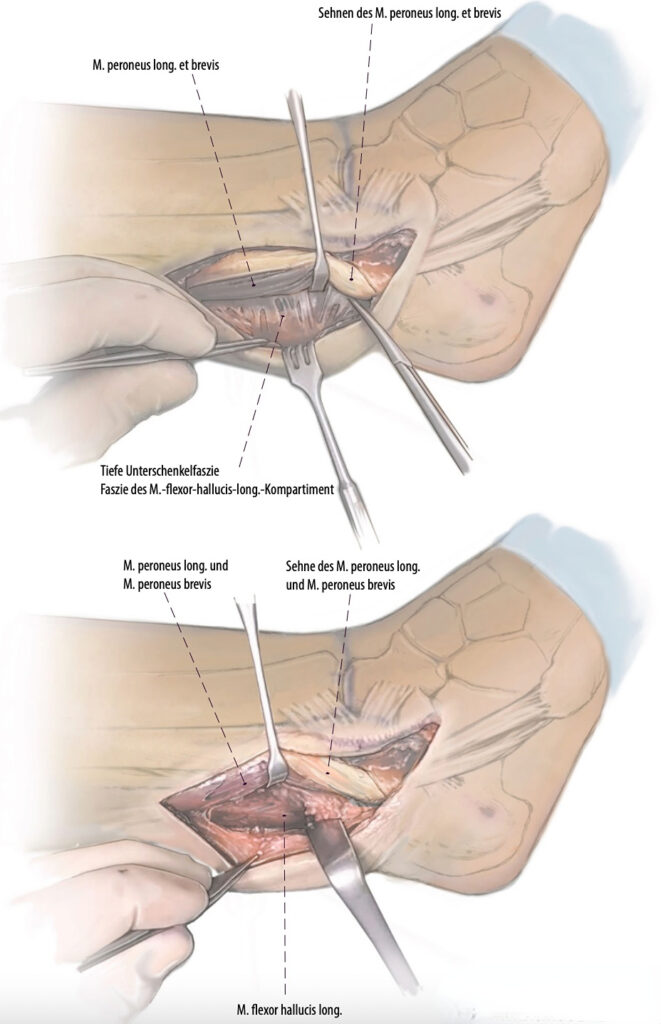
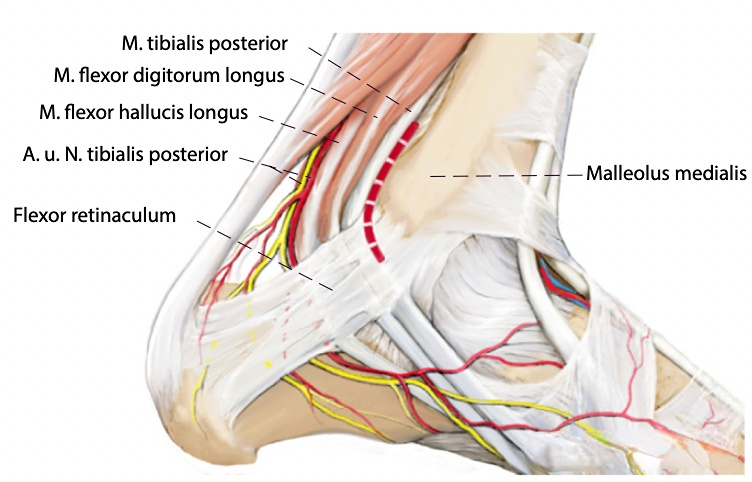
▲The peroneal tendons are retracted upward. The deep fascia of the calf is directly visible below. The flexor hallucis longus (FHL) is exposed. Care must be taken to avoid injury to the FHL throughout the procedure to avoid secondary reining deformity. The FHL and peroneal tendons are retracted, and most of the posterolateral tibia can be seen in the gap.
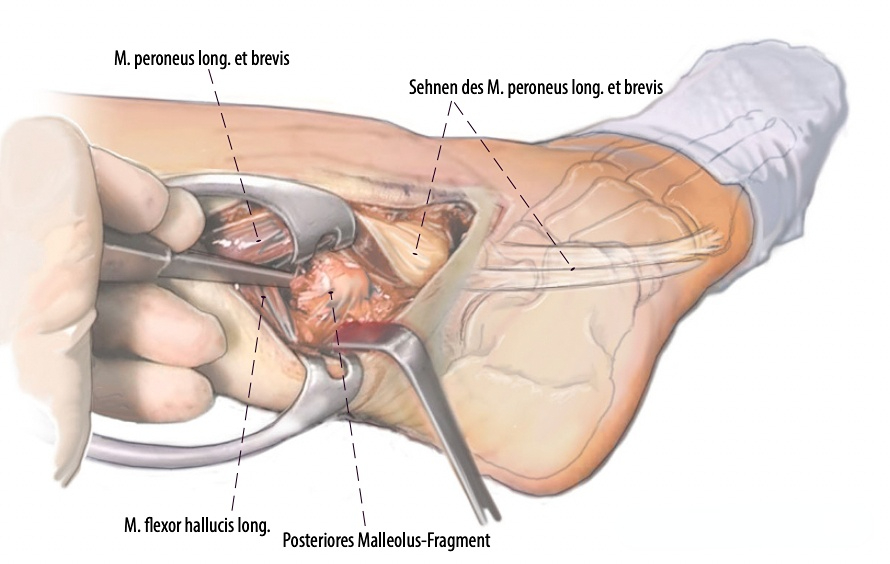
▲The posterior malleolus fracture is reduced by removing the periosteum from the fracture area while carefully protecting the posterior tibiofibular ligament and joint capsule. Exposure of the proximal fracture line is essential because it is used to reference the reduction. The fracture gap is then cleaned and small intercalated fragments are removed if necessary. In some cases, absorbable nails or the “lost pin” technique can be used to reduce and fixate large intercalated fragments.
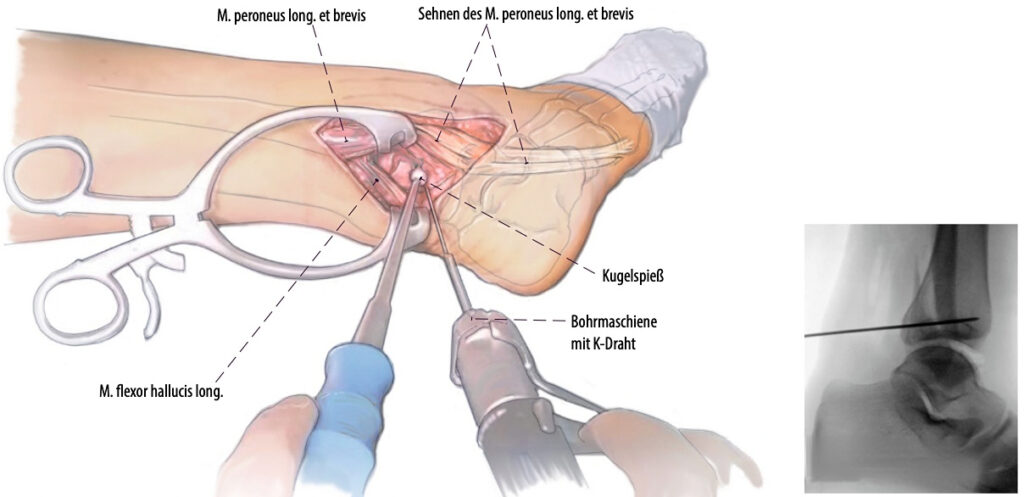
▲The picture shows a temporary fixation of the posterior malleolus fracture with a Kirschner wire after reduction. At the same time, intraoperative fluoroscopy ensures optimal reduction and Kirschner wire position.
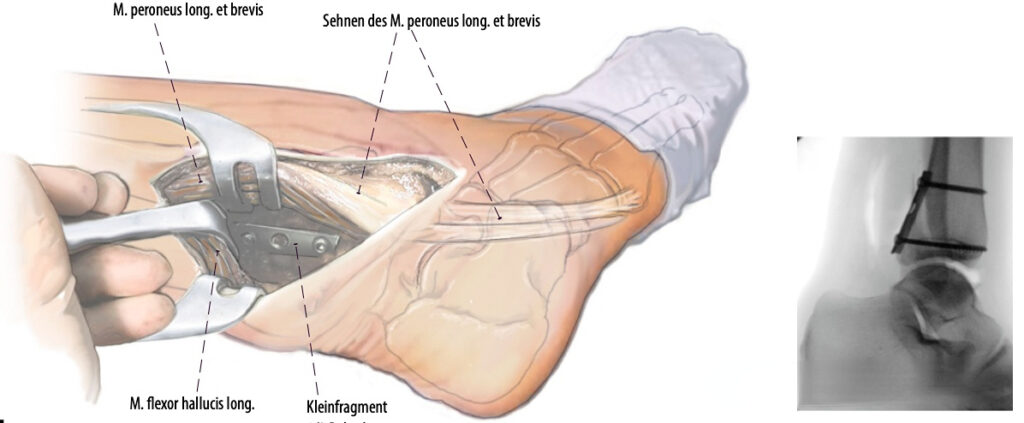
▲If the reduction is correct, a support plate (in this case, a 1/3 tubular plate) is inserted. Depending on the size and shape of the posterior malleolus fracture fragment, a plate or screws can be used for fixation. At the same time, intraoperative fluoroscopy ensures the optimal reduction and internal fixation position.
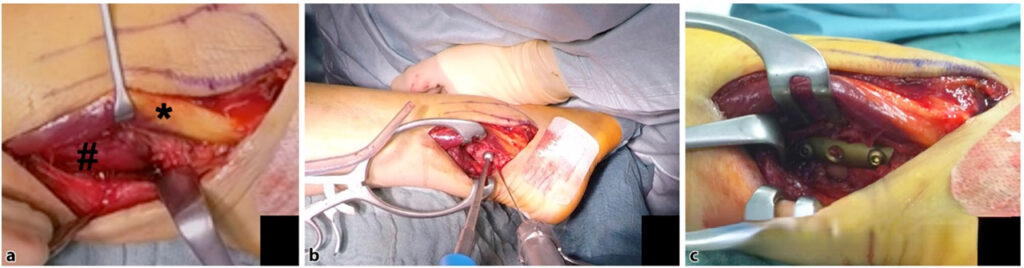
▲Intraoperative photos. (a) Incise the deep fascia of the posterior calf (peroneus tendon*; flexor hallucis longus#); (b) Anatomical reduction and temporary Kirschner wire fixation of the posterior malleolus fracture; (c) The posterior malleolus fracture is fixed with a 1/3 tubular plate.
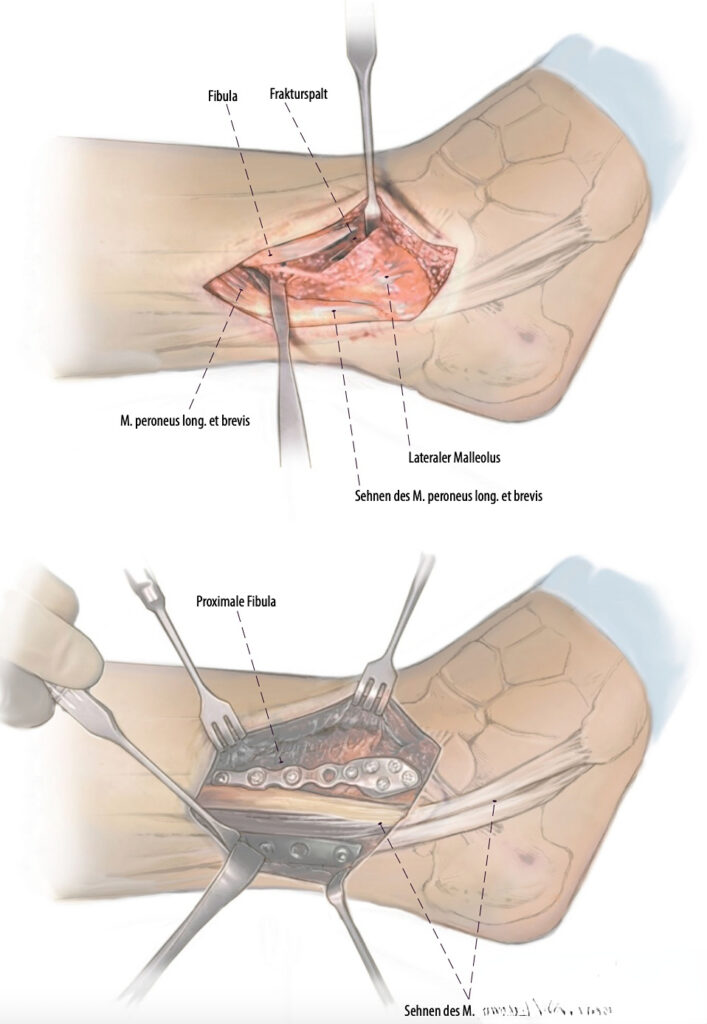
▲Treatment of the fibula: If there is a lateral malleolus fracture at the same time, it can be treated in another window of the same incision. Generally, it is necessary to expose the upper part of the peroneal tendon, the lateral malleolus, and the anterior and lateral tibia, including the Tillaux-Chaput tubercle. The fixation of the lateral malleolus fracture can be performed using a lateral anatomical plate or a posterior anti-slip plate. If a medial malleolus fracture needs to be treated, the patient is placed in the supine position.
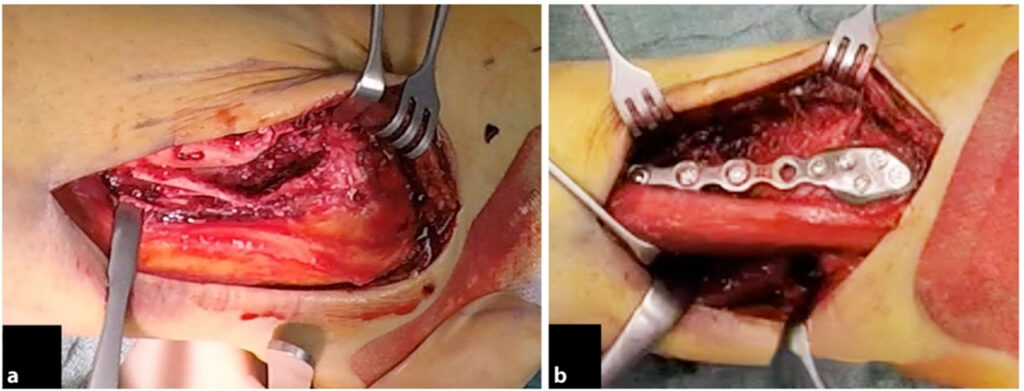
▲Intraoperative photos. (a) The lateral malleolus fracture is exposed in front of the peroneal tendon; (b) The lateral malleolus fracture is fixed using a lateral anatomical plate.
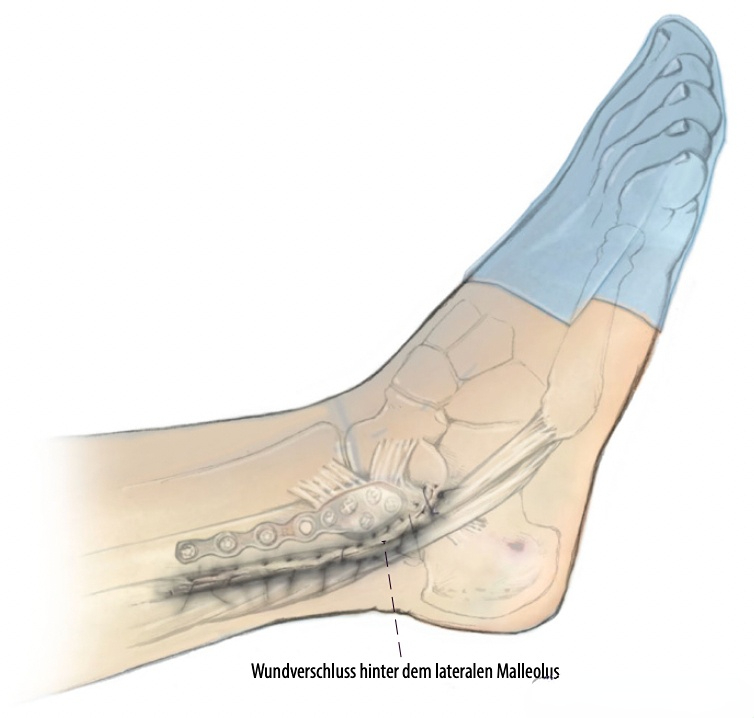
▲The wound is closed. The plate on the lateral malleolus is completely covered by the skin flap. Finally, a sterile wound dressing is applied with pressure.
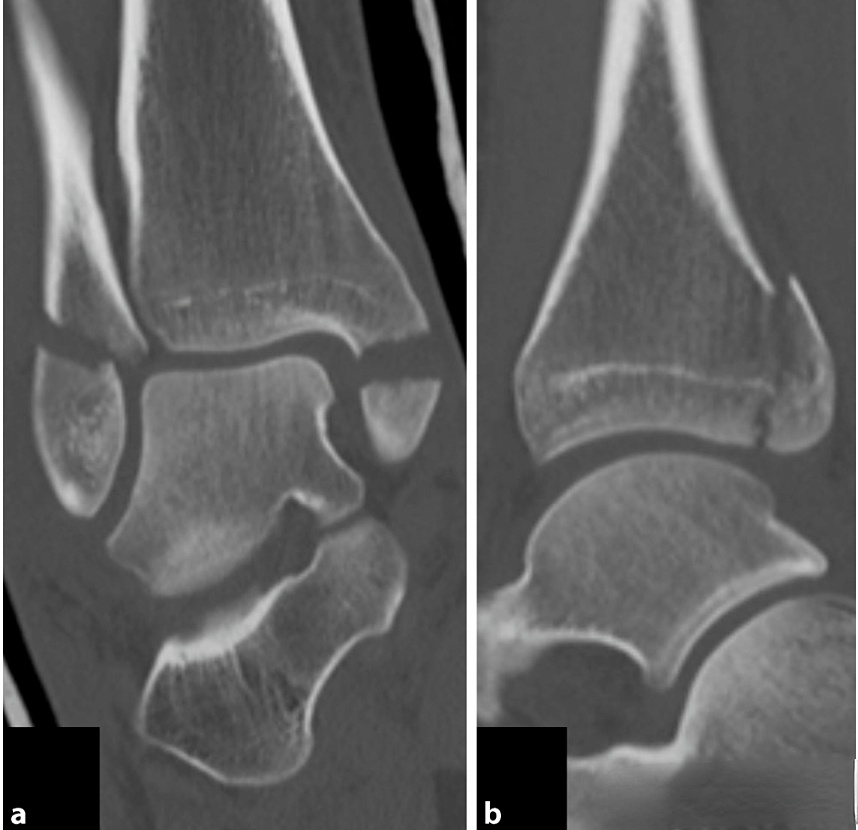
▲The figure shows the coronal (a) and sagittal (b) preoperative CT images of an AO 44-B3.2 ankle fracture.
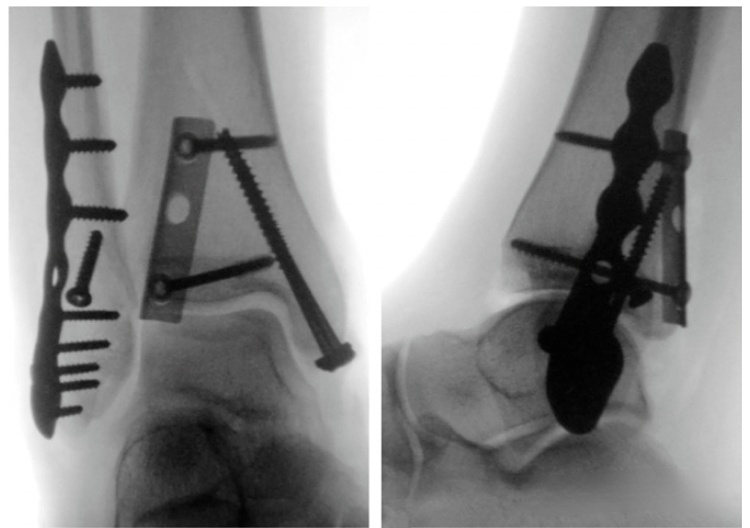
▲The picture shows the anteroposterior and lateral views of the ankle joint after reduction and fixation.

▲Figures (a) and (b) are perspective views of the ankle acupoints before and after external rotation stress testing.
▲The figure shows a combined posterolateral and posteromedial approach for complex type III or IV fractures. For posterior malleolar fractures involving the entire tibia (type III or IV fractures in the Bartoníček-Rammelt classification), anatomic reduction may not only be achieved through the posterolateral approach. It can be achieved through a combined posteromedial (red dashed line) approach.
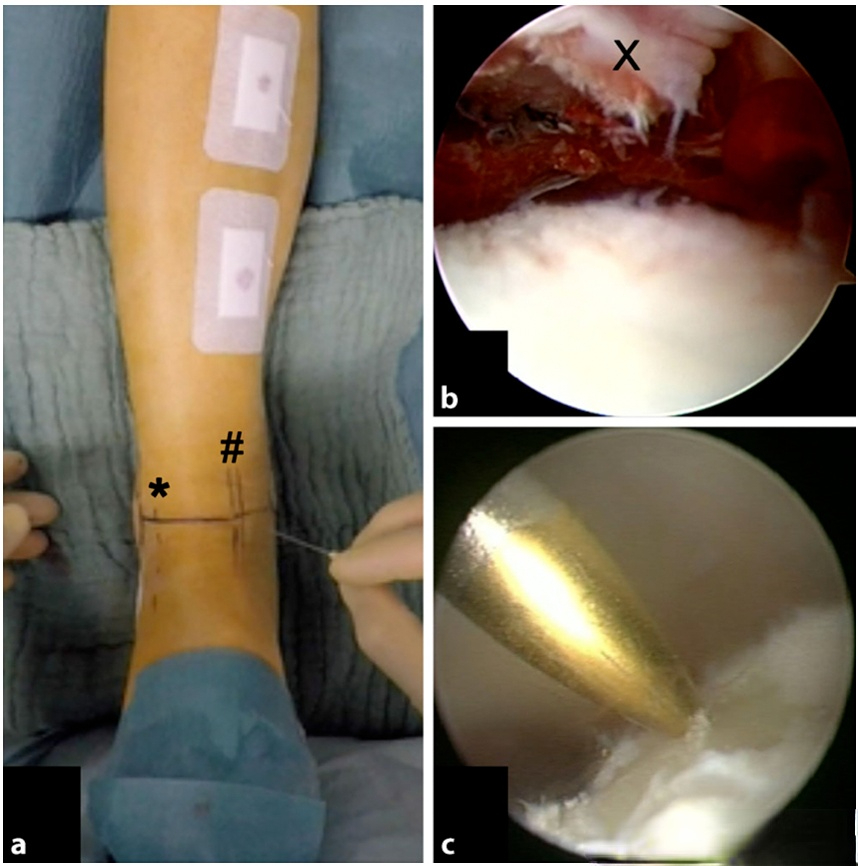
▲Ankle arthroscopy can also be performed during surgery; (a) Arthroscopic approach; (b) Cleaning of intra-articular free fractures and cartilage fragments (x); (c) Treatment of microfractures of talar cartilage injuries.
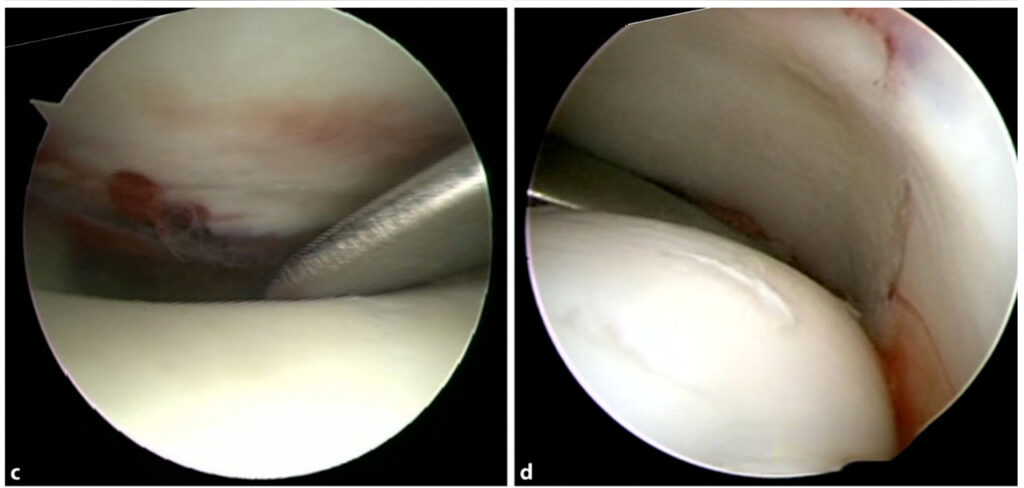
▲The figure shows the reduction effect of the posterior malleolus (c) and medial malleolus (d) under arthroscopic monitoring.
[Statement]: The concepts, technologies, and principles shared on this platform are all publicly available journals, published books, or online platform materials. The copyright belongs to the original author. The platform only organizes, summarizes, and shares them for learning reference. This platform is not responsible for the authenticity of the content and the effectiveness of the technology. The related medical behaviors generated based on the content pushed by this platform have nothing to do with the platform. Please choose carefully. If there is any infringement, please contact us to delete it.
Welcome to share, forward and like the article in the lower right corner!




