Intertrochanteric #fracture is the most common hip fracture in clinical practice and one of the three major osteoporotic fractures in the elderly. Conservative treatment requires long-term bed rest, with extremely high risks of bedsores, lung infection, pulmonary embolism, deep vein thrombosis, etc., and is difficult to care for and has a long recovery period, which brings a heavy burden to society and families. Therefore, early surgical treatment under tolerable conditions is the key to achieving good functional outcomes for hip fractures.
At present, #PFNA (proximal femoral nail anti-rotation system) internal fixation is the gold standard for surgical treatment of hip fractures, and intraoperative reduction of hip fractures to achieve positive support is the key to allowing early functional exercise (for the issue of positive and negative support for hip fractures, please refer to: Negative support VS positive support? Issues of non-anatomical reduction of hip fractures (updated version)). The intraoperative fluoroscopy field uses the AP and lateral positions to evaluate the reduction of the anterior medial cortex of the femur. However, the AP and lateral fluoroscopy methods inevitably have contradictions during the operation (i.e., the lateral position is positive and the AP position is not positive, or the lateral position is not positive and the AP position is positive). In this case, how to evaluate whether the reduction is acceptable and whether reduction adjustment is needed is a problem that bothers clinicians. To this end, scholars from Oriental Hospital and Zhongshan Hospital in China analyzed the accuracy of AP and lateral evaluation of positive and negative support under intraoperative fluoroscopy, using postoperative three-dimensional CT as the standard.
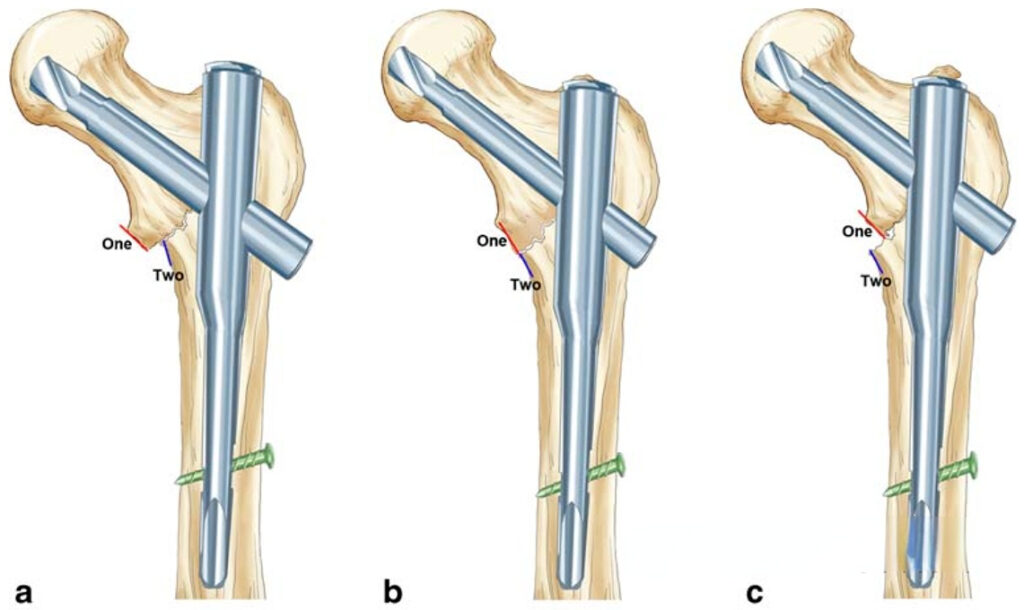
▲ The figure shows the positive support (a), neutral support (b) and negative support (c) patterns of hip fracture in the anteroposterior position.
▲ The figure shows the positive support (d), neutral support (e) and negative support (f) patterns of hip fracture in the lateral view.
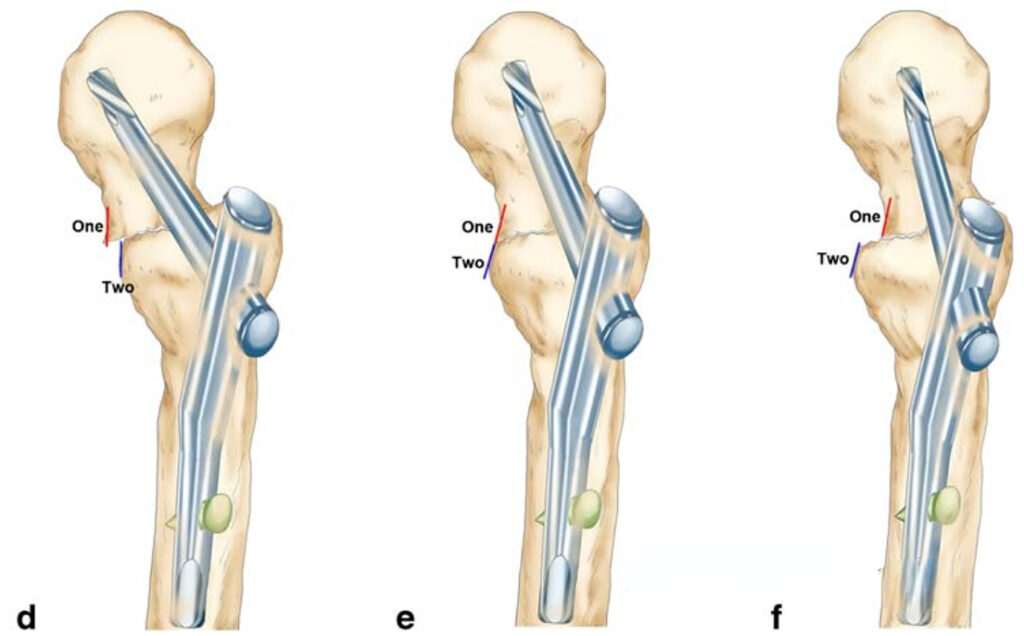
The article included the case data of 128 patients with hip fractures. The intraoperative anteroposterior and lateral radiographs were given to two doctors (younger and older) to evaluate positive support or non-positive support. Two months after the initial evaluation, they were evaluated again. The postoperative CT images were given to an experienced professor to assess the case as positive or non-positive, which was used as a standard to evaluate whether the imaging evaluations of the first two doctors were accurate. The article mainly compared:
(1) Is there a statistical difference in the evaluation results of the junior or senior doctors between the two evaluations? And the consistency between the junior and senior groups of the two evaluations, and the consistency within the two evaluations.
(2) Using the CT gold standard as a reference, which is more reliable for the reduction quality evaluation of the lateral or anteroposterior position?
Research result
In the two rounds of evaluation, with CT as the reference standard, there was no statistical difference in the sensitivity, specificity, false positive rate, and false negative rate of the reduction quality evaluated by two doctors of different seniority based on intraoperative X-ray.
- In the assessment of reduction quality, taking the first assessment as an example:
If the anteroposterior and lateral assessments are consistent (both positive or both non-positive), the reliability of predicting the reduction quality on CT is 100%;
If the anteroposterior and lateral assessments are inconsistent, the lateral assessment criteria are more reliable in predicting the reduction quality on CT.
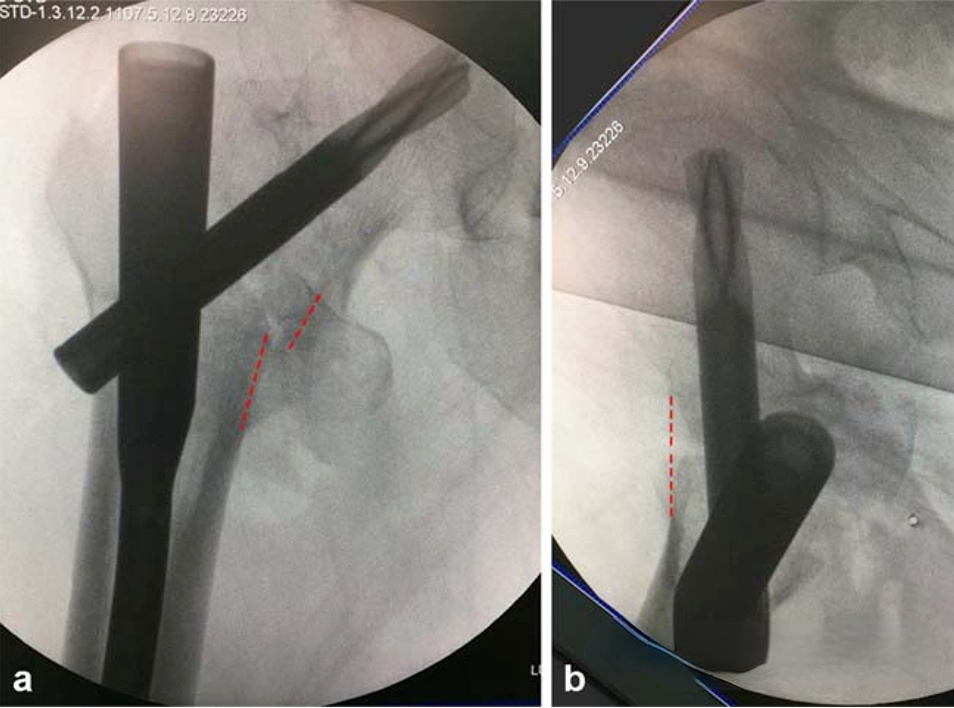
▲ The figure shows positive support in the anteroposterior view, but non-positive in the lateral view. That is, the evaluation results of the anteroposterior and lateral views are inconsistent.
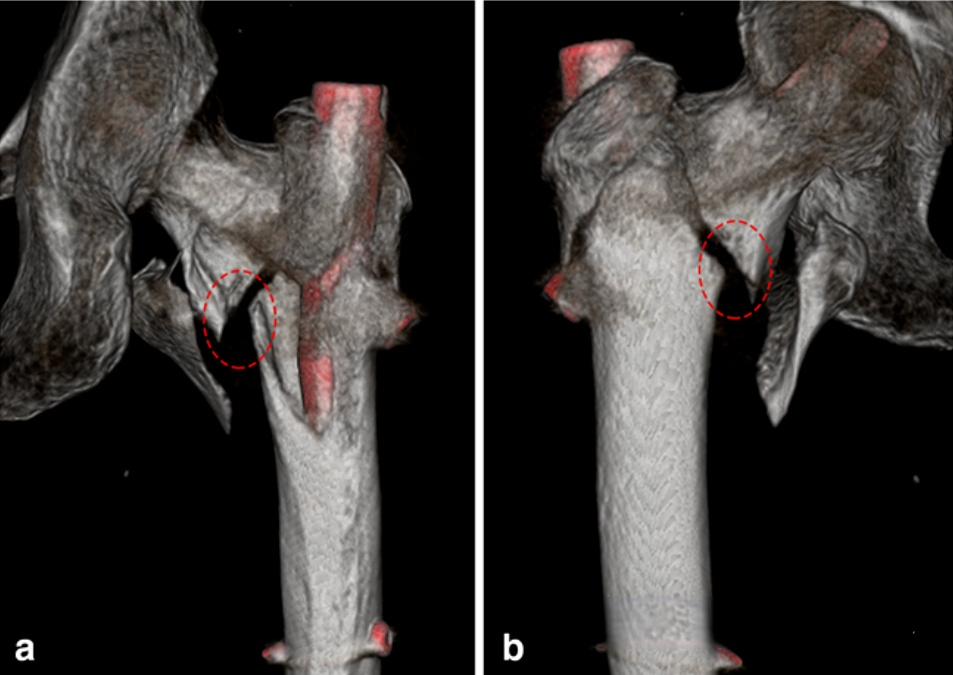
▲ Three-dimensional CT reconstruction can obtain multi-angle observation images, which can be used as a standard for evaluating the quality of reduction.
In the previous reduction standards for intertrochanteric fractures, in addition to positive and negative support, there is also the concept of “neutral” support, that is, anatomical reduction. However, due to the problem of perspective resolution and human eye recognition, the real “anatomical reduction” does not exist in theory, and there is a slight “positive” or “negative” reduction. The Zhang Shimin team of Shanghai Yangpu Hospital once published an article (I forgot the specific literature) that it is possible that intertrochanteric fractures can achieve positive support, and the functional results are better than anatomical reduction (friends who have the original text can send it to me). Therefore, combined with this article, during surgery, the intertrochanteric fracture should be made to achieve positive support as much as possible. If both the anteroposterior and lateral positions are achieved, the reduction is optimal. If the lateral position achieves positive support and the anteroposterior reduction is unsatisfactory, there may be no need for “unnecessary” readjustment.
【Article】Jia X, Zhang K, Qiang M, Chen Y. The accuracy of intra-operative fluoroscopy in evaluating the reduction quality of intertrochanteric hip fractures. Int Orthop. 2020 Jun;44(6):1201-1208.
【Note】: The concepts, technologies, and principles shared on this platform are all publicly available journals, published books, or online platform materials. This platform is not responsible for the authenticity of the content and the effectiveness of the technology. The related medical behaviors generated based on the content pushed by this platform have nothing to do with the platform. Please choose carefully.
Welcome to share, forward and like the article in the lower right corner!




