Intramedullary nail fixation is the gold standard for tibial shaft fractures. It has excellent biomechanical advantages with axial fixation and minimally invasive placement. The infrapatellar approach requires extreme knee flexion and is not suitable for some special types of fractures, such as proximal 1/4 tibial fractures, multiple tibial fractures, extreme distal fractures, infrapatellar soft tissue contusion, and patients with limited knee flexion. The suprapatellar approach can be placed with the knee slightly flexed, which has advantages in the above-mentioned types of fractures.
After the fracture heals, most domestic patients may choose to remove the internal fixation. In clinical work, the suprapatellar intramedullary nail of the tibia is usually removed through the infrapatellar approach, which may be due to the following reasons:
The suprapatellar approach is deep, and it is difficult to find the tail cap of the intramedullary nail;
It is necessary to pass through the knee joint, which may damage the patellofemoral joint cartilage.
The infrapatellar approach can usually expose the tail cap more clearly and clean the ingrown soft tissue and callus, but another incision is required below the patella, which increases additional scars. For this reason, domestic scholars have tried to remove the intramedullary nail from the original suprapatellar incision and have been successful:
There are two problems to be solved when removing intramedullary nails from the suprapatellar approach:
One is how to accurately find the tail cap of the intramedullary nail;
The other is how to clean the soft tissue and callus that the tail cap has grown into.
First, find the needle insertion point of the tibial intramedullary nail and locate the tail cap. The author uses a 3.2mm guide needle and confirms it through intraoperative fluoroscopy (under the current circumstances, is it a bit of a luxury to remove the nail with a guide needle?):
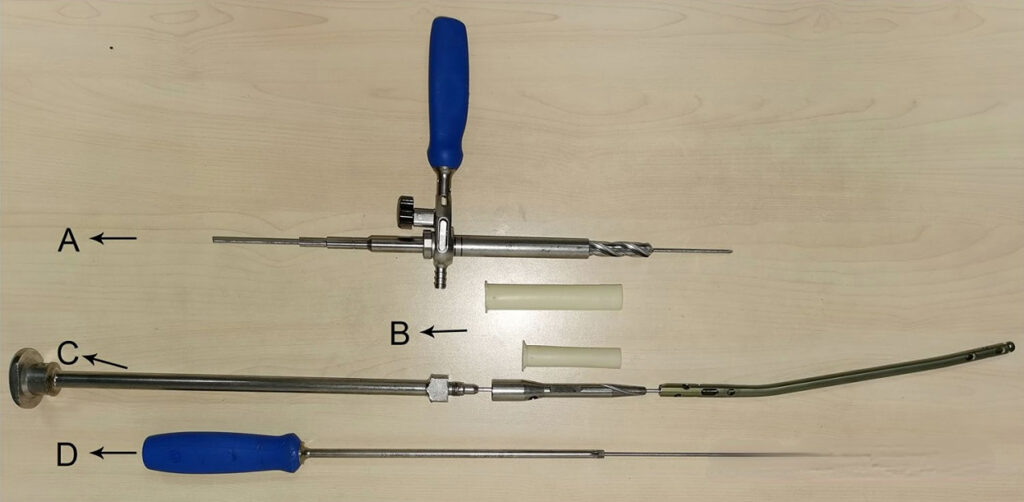

The patellofemoral joint usually becomes scarred due to the original surgical trauma, resulting in a tight patellofemoral joint. It may be difficult to directly insert the protective sleeve, or it may be difficult to move after insertion (stuck in the intercondylar notch of the femur). However, it is relatively simple to insert the protective sleeve through a guide needle. After inserting the sleeve, use a drill bit to remove the callus and soft tissue around the tail cap, and use a hollow screwdriver to remove the tail cap.

After the tail cap is removed, the guide pin is inserted. After the nail removal tool is screwed into the tail of the intramedullary nail and firmly fixed, the distal locking screw is removed and the main nail of the intramedullary nail is removed by hammering. Note that the locking screw at the proximal end of the intramedullary nail can be removed first in the first step, but the distal locking screw must be removed after the tail cap is removed and the nail removal tool is fixed to the tail of the intramedullary nail to avoid axial movement or rotation of the intramedullary nail during the operation.

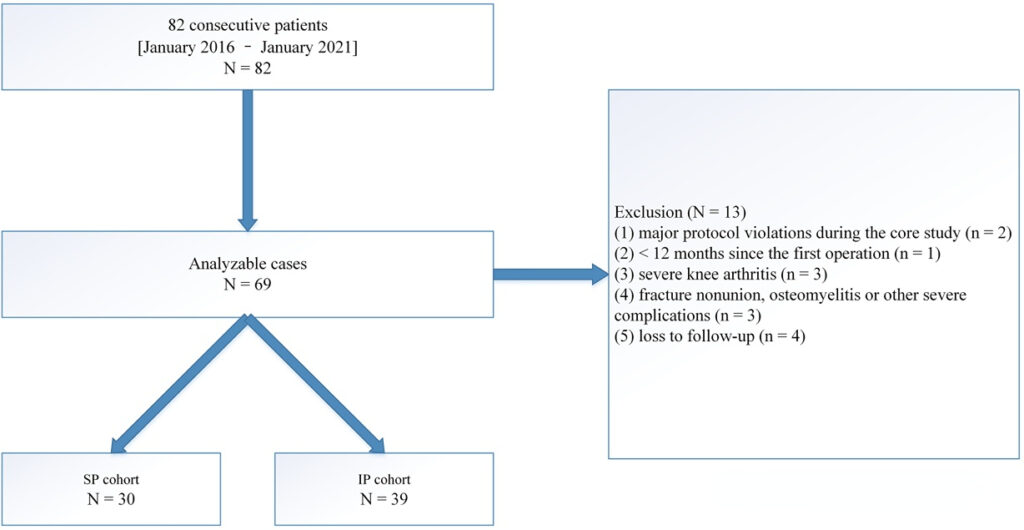
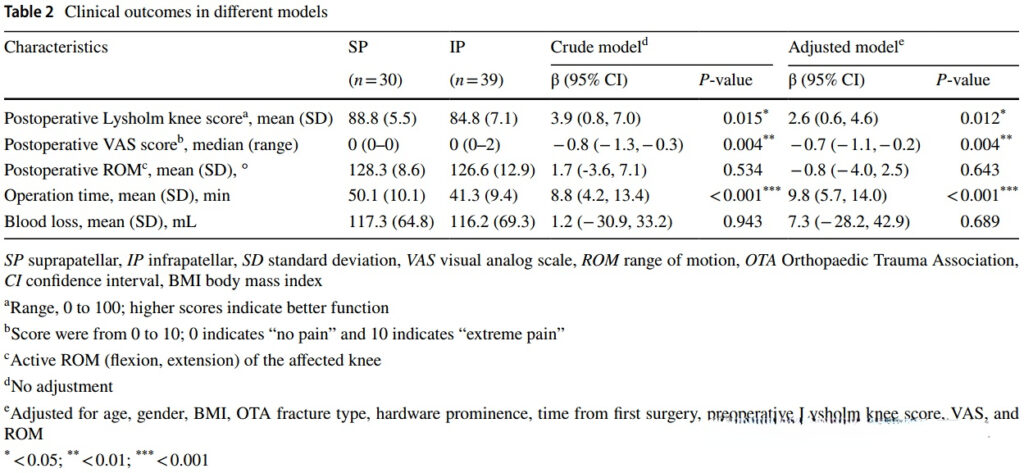
In this study, the authors included 69 patients, of whom 30 were removed suprapatellar and 39 were removed infrapatellar. The suprapatellar group had a higher Lysholm score and a lower VAS score.
After the study was published, doctors from the First People’s Hospital of Xiaoshan District, Hangzhou, published a related question in the same journal:
The main points include the following:
Does the suprapatellar group increase the number of fluoroscopy, which is crucial for orthopedic surgeons;
How to calculate and evaluate the amount of bleeding in the two groups?
Does the suprapatellar group increase the patellofemoral joint cartilage damage, and is there an MR review assessment?
What do you think about this?
[Statement]: The concepts, technologies, and principles shared on this platform are all publicly available journals, published books, or online platform materials. The copyright belongs to the original author. The platform only organizes, summarizes, and shares them for learning reference. This platform is not responsible for the authenticity of the content and the effectiveness of the technology. The related medical behaviors generated based on the content pushed by this platform have nothing to do with the platform. Please choose carefully. If there is any infringement, please contact us to delete it.




