General Concepts :
1. Epinephrine Use: While historically feared due to vasoconstriction risk, epinephrine can be safely used in digital blocks at diluted concentrations (1:200,000 or 1:400,000), with careful aspiration, and potential phentolamine reversal (0.5% solution). Monitor perfusion closely.
2. Betadine and Bone: Betadine, while an effective antiseptic, has been shown to be cytotoxic to osteoblasts in vitro. Irrigate exposed bone thoroughly after using Betadine to minimize potential negative impact on healing.
3. Imaging Interpretation: Advanced imaging (MRI, CT) offers valuable information, but clinical correlation is paramount. Don’t solely rely on imaging findings; integrate them with history, physical exam, and patient goals.
4. Gilula’s Lines: Disruptions in the smooth arcs of carpal bones on PA/AP views suggest carpal instability. However, minor variations can be normal. Clinical examination is crucial to determine if instability is present.
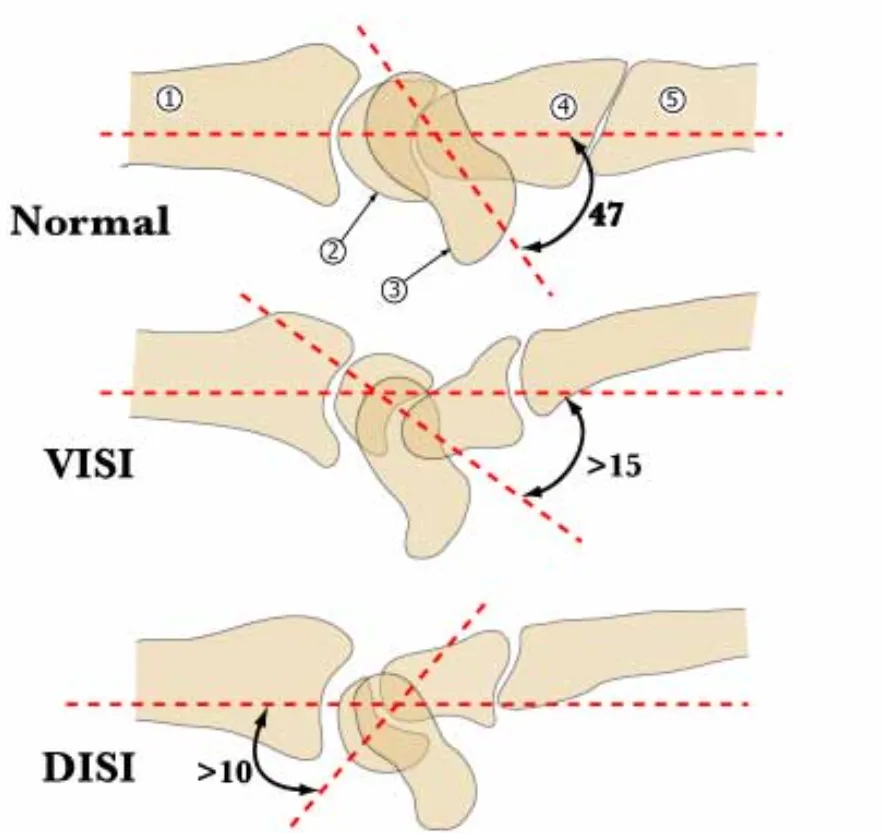
5. DISI/VISI: Dorsal Intercalated Segment Instability (DISI) and Volar Intercalated Segment Instability (VISI) describe lunate posture on lateral radiographs. While DISI reliably indicates scapholunate ligament disruption, VISI can be a normal variant or indicate lunotriquetral ligament injury or generalized ligamentous laxity.
6. Scaphoid Views: The ulnar deviation view is commonly obtained for suspected scaphoid fractures, but its sensitivity is limited (~64%). MRI or CT are more sensitive for occult fractures.
7. Zero Rotation Views: Essential for accurate ulnar variance assessment and evaluating DRUJ congruency. Ensure proper patient positioning for reliable measurements.
8. Tendon Retraction: Avoid pulling distally and suturing retracted flexor or extensor tendons to cover bone, as this compromises tendon gliding and function. Cover exposed bone with skin grafts or flaps.
9. Nerve Transection: All nerve transections result in neuroma formation. Minimize symptom potential by transecting the nerve sharply under tension to allow retraction into a well-padded area away from the surgical scar and potential mechanical irritation.
10. Zone II Flexor Tendon Repair: Modern techniques and early active motion protocols have improved outcomes, but results are still variable. Meticulous surgical technique, appropriate patient selection, and careful postoperative monitoring of therapy are crucial.
11. Flexor Tendon Repair Strength: The repair site is weakest in the first 4 weeks after surgery, especially if immobilized. Emphasize protected mobilization with early active motion protocols to maximize healing and minimize adhesion formation.
12. Edema Control: Crucial for successful tendon healing and rehabilitation. Implement elevation, compression, and early active motion to minimize edema.
13. Tendon Transfer Strength: Expect a loss of approximately one MRC grade of strength in the transferred muscle. Choose a donor muscle with sufficient strength to perform the desired function after transfer.
14. Tendon Transfer Amplitude: Match excursion of the donor and recipient tendons. Use the tenodesis effect to augment amplitude if needed.
15. Tendon Transfer Synergy: Transfers are more effective when the transferred muscle’s action is synergistic with the function it replaces.
16. Arthrodesis: Avoid fusion if possible to preserve joint mobility and the tenodesis effect. Consider the impact of fusion on adjacent joints.
17. Tenosynovitis vs. Tendon Rupture: Differentiate by evaluating if the patient can actively maintain joint position once passively placed.
18. Septic Arthritis vs. Crystalline Arthropathy: Arthrocentesis is mandatory for diagnosis. Don’t exclude infection based on the presence of crystals alone, as both conditions can coexist.
19. Zone of Injury: The zone of injury in acute trauma extends beyond the visible wound due to perivascular inflammation and potential for delayed microvascular thrombosis. Consider this when choosing recipient vessels for free flap anastomosis and prioritize vessel selection outside the zone.
20. Doppler Allen Test: A critical component of the vascular examination for suspected arterial injury. Consistently perform a Doppler Allen test to assess radial and ulnar artery patency.
21. Angiography: Not routinely indicated for acute, single-level penetrating arterial injuries when the site of injury is known. Consider for complex injuries, suspected embolic events, or potential for thrombolytic intervention.
Specific Conditions:
Chronic Pain Syndromes:
1. CRPS Diagnosis: CRPS is a clinical diagnosis. There is no pathognomonic test. The diagnosis requires the presence of disproportionate pain and at least two of the following: stiffness, delayed functional recovery, trophic changes, and autonomic dysfunction.
2. CRPS vs. Neuropathic Pain: CRPS is a type of neuropathic pain, but it differs from other neuropathic pain syndromes by the presence of pain spreading beyond the expected nerve distribution and by the presence of autonomic dysfunction.
3. CRPS Treatment: Early recognition and aggressive multidisciplinary intervention are key for optimal outcome. Treatment should address sympathetically maintained pain, edema, functional impairment, and any identifiable nociceptive or neuropathic contributions.
4. “Hot” vs. “Cold” CRPS: These represent distinct physiological stages of microvascular perfusion associated with CRPS. Treatment should be tailored to each stage. “Hot” CRPS is characterized by edema, increased sweating, and hyperalgesia. “Cold” CRPS is characterized by atrophy, pain with cold intolerance, and diminished sweating.
Tendon:
1. Trigger Finger Injection: While subcutaneous injection of corticosteroid can be effective, intratendinous injection should be avoided due to the risk of tendon rupture.
2. Intersection Syndrome: Pain is frequently noted over the first dorsal compartment (APL and EPB) at the wrist, but the tenosynovitis actually affects the second dorsal compartment (ECRL and ECRB) under the extensor retinaculum.
3. ECU Tendonitis: Painful snapping of the ECU tendon with forearm pronation/supination suggests ECU instability due to a subsheath tear.
4. FCR Tendonitis: A diagnosis of exclusion. Thoroughly rule out other causes of volar radial wrist pain before making this diagnosis.
5. Lateral vs. Medial Epicondylitis: Consider radial tunnel syndrome in lateral epicondylitis (pain with resisted middle finger extension) and ulnar neuritis in medial epicondylitis (pain with resisted wrist flexion, pronation, and ulnar deviation).
6. Chronic EPL Rupture: Frequently caused by attritional rubbing against Lister’s tubercle. Evaluate for predisposing factors such as rheumatoid arthritis, scapholunate instability, or previous distal radius fracture.
7. Chronic ECU/EDQ Rupture: Rheumatoid arthritis with caput ulnae syndrome (dorsal subluxation of the ulna) is a common cause for these attritional ruptures.
Arthritis:
1. Seropositive vs. Seronegative Arthritis: The presence or absence of rheumatoid factor in the blood distinguishes these two broad categories of inflammatory arthritis. Seropositive arthritis includes rheumatoid arthritis, while seronegative arthritis includes psoriatic arthritis, ankylosing spondylitis, reactive arthritis, and enteropathic arthritis.
2. Psoriatic Arthritis: DIP joint involvement, nail changes (pitting, onycholysis), and dactylitis are common. Treatment often requires a combination of medical management and surgical intervention.
3. Systemic Lupus Erythematosus (SLE): Hand deformities mimic RA, but joint involvement is due to soft tissue laxity, tendon subluxations, and capsular laxity, rather than articular destruction. Radiographs typically do not show erosions or joint space narrowing.
4. Scleroderma: Skin fibrosis, Raynaud phenomenon, and digital ulcerations are prominent features. Surgery should be avoided if possible due to a high risk of wound healing complications.
5. Acute Gout: Can mimic septic arthritis, especially in the wrist, with rapid onset of pain, erythema, and swelling. Arthrocentesis is crucial for differentiation.
6. Chronic Gout: Tophi (deposits of urate crystals) can cause erosions on both sides of the joint, typically with sclerotic borders and overhanging margins. Late findings include joint space narrowing and destruction.
7. Chronic CPPD: Often presents as a SLAC-like wrist collapse with chondrocalcinosis (linear calcifications at the articular surface). Treatment options include those used for SLAC wrist.
8. Septic Arthritis: A joint-threatening emergency. Requires urgent arthrotomy, drainage, irrigation, and IV antibiotics. Delayed treatment can result in permanent cartilage damage, joint destruction, and loss of function.
9. Juvenile Idiopathic Arthritis: Several subtypes with distinct clinical presentations and treatment considerations. Unlike adult rheumatoid arthritis, growth abnormalities are common and can affect the choice of treatment.
10. Trapeziometacarpal Arthritis: Radiographic findings do not always correlate with symptoms. Patients may have severe arthritis on radiographs but be asymptomatic. Conversely, patients with minimal radiographic changes may experience disabling pain.
11. Carpal Boss: A bony prominence at the base of the second or third metacarpals, often mistaken for a fracture. Use carpal boss views (lateral with supination and flexion) to accurately diagnose.
Vascular Conditions :
1. Hemangioma vs. Venous Malformation: Hemangiomas are true tumors with rapid growth in infancy followed by involution. Venous malformations are not true tumors and grow commensurately with the child.
2. Hypothenar Hammer Syndrome: Caused by repetitive trauma to the ulnar artery in the hypothenar eminence, leading to thrombosis, aneurysm formation, and distal embolization. Has a strong association with smoking.
3. Arterial Aneurysm: A permanent localized dilatation of the artery 50% or greater above normal diameter. Consider the possibility of distal embolization as a presenting sign, especially for ulnar artery aneurysms.
4. Digital Artery Aneurysm: Often mistaken for a soft tissue mass, especially in the fingertip. Transverse mobility but lack of longitudinal mobility is a key differentiating sign.
Other:
1. Mutilating Hand Injuries: These are combined injuries involving multiple structures with a poorer prognosis than isolated injuries. Requires a systematic approach to evaluation and treatment.
2. Compartment Syndrome: Can occur with open wounds. Pain on passive stretch is the most reliable clinical sign for early diagnosis and is present even before neurological deficits.
3. Informed Consent: The informed consent discussion should ideally occur in the office, not immediately before surgery. Document the discussion thoroughly in the office note. Ensure that patients understand the risks and benefits of the proposed procedure, alternative treatment options, and the risks of refusing treatment.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. In order to ensure the “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!




