Fracture-related infections (FRIs) are a complex and challenging complication in orthopedic surgery. Often confused with prosthetic joint infections (PJIs), FRIs present distinct obstacles that require a nuanced approach. Here are some key points to clarify common misunderstandings:
FRI vs. PJI: Understanding the Differences
1. Unique Challenges:
While both FRIs and PJIs involve biofilm formation, FRIs are complicated by factors like the presence of a fracture, ongoing bone healing, and soft tissue injuries. These elements make treatment more complex than in PJIs.
2. Treatment Goals Differ:
In PJIs, the primary goal is to eradicate infection, often requiring implant removal. However, in FRIs, the focus is on fracture healing and preventing chronic osteomyelitis. In some cases, complete infection eradication may not be immediately necessary, and suppressive antibiotics can serve as a temporary measure until implant removal is viable.
Time is Not Everything:
3. Onset Time Can Be Misleading:
Classifying FRIs based solely on the time since injury is misleading. While early infections may involve more aggressive bacteria and late infections less virulent strains, this distinction is not always reliable. Tailored treatment based on the infection’s specific characteristics is crucial.
Diagnosis is Tricky:
4. Overlapping Symptoms:
Diagnosing FRIs can be difficult because clinical symptoms may overlap with normal fracture healing. A thorough examination and a high level of suspicion, especially in high-risk patients, are essential.
5. Inflammatory Markers Need Context:
Markers like ESR, CRP, and white blood cell count can be elevated due to the fracture itself. However, a secondary rise after an initial decrease, or an unexplained elevation, is more indicative of infection.
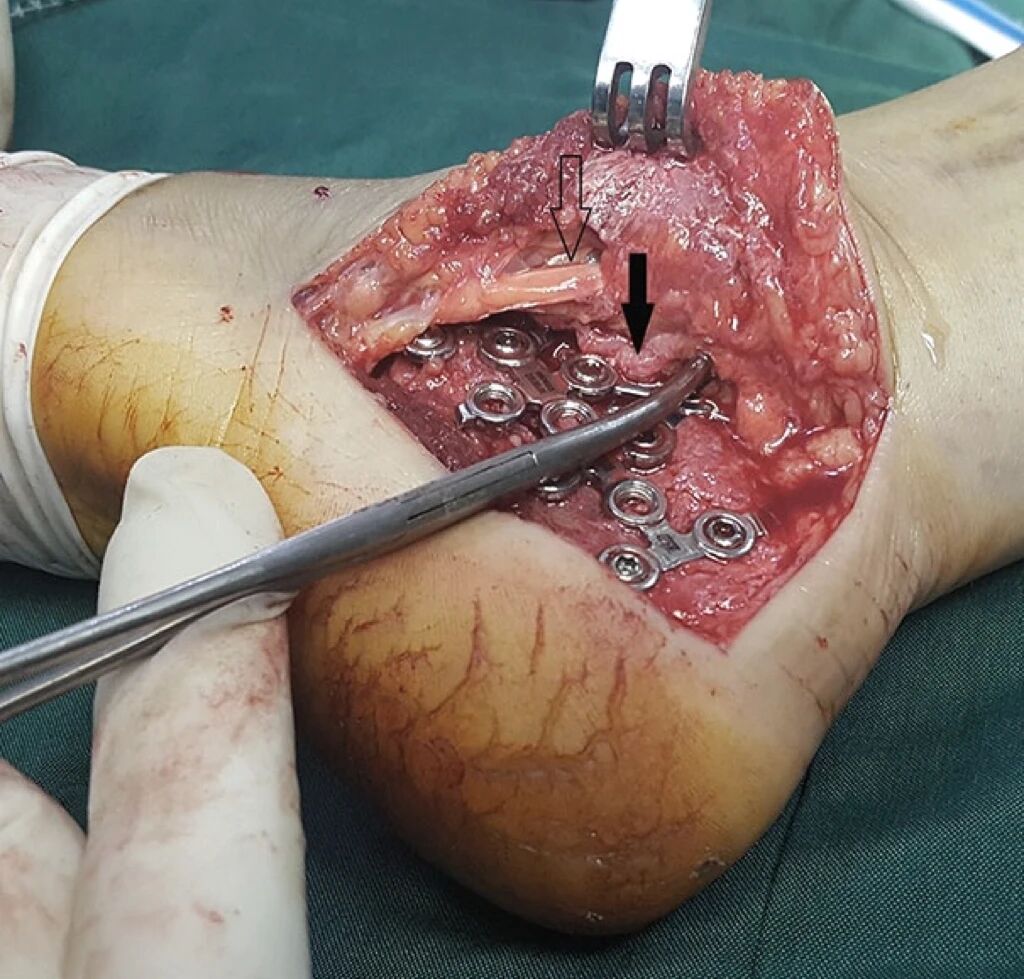
6. Deep Cultures are Key:
Taking intraoperative deep tissue cultures is the gold standard for diagnosing FRIs. Superficial swabs are unreliable due to contamination risks. Multiple deep samples from different locations around the fracture and implants improve diagnostic accuracy.
7. Sonication Still Debated:
While sonication can help dislodge bacteria from implants, improving culture yield, its added value in FRI diagnosis is still under investigation. More research is needed.
8. Histopathology Provides Clues:
Histopathological examination of deep tissue biopsies can be especially helpful in chronic cases. The presence of polymorphonuclear neutrophils (PMNs) strongly suggests infection. Combining this with microbiology results increases diagnostic precision.
9. PCR Limitations:
Though PCR can rapidly detect bacterial DNA, it cannot distinguish between living and dead bacteria, which can lead to false positives. Its role in diagnosing FRIs remains controversial and requires further study.
Prevention and Treatment Strategies:
10. Early Soft Tissue Coverage is Critical:
Prompt soft tissue coverage of open fractures is key to preventing FRIs. Ideally, wound closure should happen within 72 hours, and no later than 7 days post-injury. Delays significantly increase the risk of infection.
11. Local Antibiotics Show Promise:
Delivering antibiotics directly to the fracture site shows promise, but optimal drug choices, dosages, and delivery methods need further research.
12. Biodegradable Carriers Offer Advantages:
Biodegradable materials like calcium sulfate and bioactive glass offer a superior alternative to traditional PMMA for delivering local antibiotics. They provide sustained release, eliminate the need for implant removal, and don’t hinder bone healing.
13. Bacteriophage Therapy – A Potential Weapon:
Bacteriophage therapy, which uses viruses to target bacteria, could be a game-changer in treating FRIs. However, its safety, efficacy, and optimal dosing require more investigation.
A Team Effort:
14. Multidisciplinary Approach is Essential:
Managing FRIs effectively requires a multidisciplinary team of orthopedic surgeons, infectious disease specialists, microbiologists, and plastic surgeons. This collaborative approach ensures comprehensive care, appropriate antibiotic use, and optimized surgical strategies.
15. Individualized Treatment Plans are Key:
No single treatment fits all FRIs. Factors like fracture type, infection severity, patient health, and available resources should guide decisions about implant retention, antibiotic choice, and treatment duration.
Ongoing Challenges:
16. Outcome Measurement Needs Improvement:
Currently, there is a lack of standardized outcome measures specific to FRIs. Developing reliable tools to evaluate treatment effectiveness is critical for improving patient care.
Conclusion:
Fracture-related infections are a complex and often misunderstood complication in orthopedic surgery. A multifaceted approach involving accurate diagnosis, timely intervention, and a personalized treatment plan is essential for successful outcomes. Continued research into innovative therapies like bacteriophages and biodegradable carriers will be key to advancing treatment strategies.
Meta Description:
Learn the 15 most misunderstood points about fracture-related infections (FRIs), including their diagnosis, treatment, and prevention strategies. Discover how FRIs differ from PJIs and why a multidisciplinary approach is essential for effective management.
For more detailed guidelines on FRI management, visit the AO Trauma Foundation.
Disclaimer:
This article and all articles on this website are for reference only by medical professionals; specific medical problems should be treated promptly. To ensure “originality” and improve delivery efficiency, some articles on this website are AI-generated and machine-translated, which may be inappropriate or even wrong. Please refer to the original English text or leave a message if necessary. Copyright belongs to the original author. If your rights are violated, please contact the backstage to delete them. If you have any questions, please leave a message through the backstage, or leave a message below this article. Thank you!
Like and share, your hands will be left with the fragrance!